feetcorrector
The #1 Hack to Instantly Reduce Swelling in Your Feet
The #1 Hack to Instantly Reduce Swelling in Your Feet
Have your feet ever felt swollen? Swelling can make your feet feel uncomfortable and heavy. It can happen if you stand for too long, it’s hot outside, or if you eat a lot of salty foods.
Luckily, there’s a simple trick that can help: elevating your feet. This blog post will explain how to do it and share some extra tips to keep your feet feeling good.
Why Do Feet Swell?
Feet can swell for different reasons. Here are a few common ones:
- Standing or Sitting Too Long: If you stay in one spot for a long time, blood can pool in your feet and make them swell.
- Hot Weather: When it’s hot outside, your blood vessels can expand, causing fluid to build up in your feet.
- Eating Too Much Salt: Foods that are high in salt can make your body hold on to extra water, which can cause swelling.
- Health Issues: Sometimes, health problems like heart disease or pregnancy can lead to swollen feet.
The Hack: Elevating Your Feet
One of the easiest ways to reduce swelling is to elevate your feet. Here’s how you can do it:
- Find a Comfortable Place: Lay down on a couch or bed and grab a few pillows.
- Put Your Feet Up: Place the pillows under your feet so they are higher than your heart. Try to get them at a 30-degree angle.
- Relax for a While: Keep your feet elevated for about 15 to 30 minutes. This helps the extra fluid in your feet move back toward your heart.
When you lift your feet up, gravity helps the fluid leave your feet, making them feel better quickly!
More Tips to Reduce Foot Swelling
In addition to elevating your feet, here are some other easy things you can do to help with swelling:
- Drink Plenty of Water: Staying hydrated helps your body get rid of extra salt and water.
- Watch Your Salt Intake: Eating less salt can help stop your body from holding on to water.
- Wear Compression Socks: These special socks help keep blood moving in your legs and feet.
- Do Gentle Exercise: Activities like walking or swimming can help keep blood flowing and prevent swelling.
- Use a Cold Compress: Putting a cold pack on your feet for 10-15 minutes can help reduce swelling.
- Massage Your Feet: Gently rubbing your feet can also help move the fluid around and make them feel better.
Conclusion
Swollen feet can be uncomfortable, but elevating them can give you quick relief. Pair this with drinking water, eating less salt, and staying active for better foot health. Remember, while swelling is often normal, always listen to your body. If something doesn’t feel right, talk to a healthcare provider. Your feet work hard for you, so give them the care they deserve!
A Comprehensive Guide: Neem Oil Nail Fungus Treatment

Nail fungus, medically known as onychomycosis, is a common and stubborn condition that affects millions of people worldwide. Characterized by thickened, discolored nails, nail fungus can be unsightly and even painful if left untreated. While there are various treatments available, one natural remedy that has gained attention is neem oil. In this guide, we’ll look into the effectiveness of neem oil nail fungus treatments and explore how to use it effectively!
Understanding Nail Fungus
Before we discuss neem oil as a treatment, let’s first understand what nail fungus is and how it develops. These infections are typically the result of dermatophytes or yeast, which thrive in warm, moist environments.
The nails provide an ideal environment for fungal growth, especially toenails, as they are often confined within shoes, creating a warm and damp environment that promotes fungal proliferation. Factors such as poor foot hygiene, wearing tight or non-breathable shoes, and walking barefoot in public places like swimming pools and locker rooms can increase the risk of developing nail fungus.
Nail fungus typically begins as a small white or yellow spot under the tip of the nail and gradually spreads deeper into the nail bed. As the infection progresses, the nail may become thickened, brittle, discolored (often yellow or brown), and may emit a foul odor. In advanced stages, the nail may become distorted in shape and separate from the nail bed, causing pain and discomfort.
Understanding the underlying causes and symptoms of nail fungus is crucial for effective treatment and prevention. By recognizing the risk factors and early signs of infection, individuals can take proactive measures to protect their nails and seek appropriate treatment options, such as neem oil, to combat nail fungus effectively.
Neem Oil: Nature’s Antifungal Remedy
Neem oil, derived from the seeds of the neem tree (Azadirachta indica), has a rich history of medicinal use in various traditional healing systems, including Ayurvedic medicine. For centuries, neem oil has been revered for its versatile therapeutic properties, earning it the title of “nature’s pharmacy.”
In Ayurvedic and traditional medicine practices, neem oil is prized for its potent antifungal, antibacterial, and anti-inflammatory properties, which have been extensively documented through both traditional knowledge and modern scientific research. These properties make neem oil a promising option for combating a wide range of ailments, including nail fungus.
The antifungal action of neem oil is attributed to several bioactive compounds found in the oil, including nimbidin, nimbin, and azadirachtin. These compounds exhibit strong inhibitory effects against fungal growth and replication, targeting the underlying cause of nail fungus infection. Additionally, neem oil’s antibacterial properties help prevent secondary bacterial infections that may exacerbate nail fungus symptoms.
Neem oil possesses significant anti-inflammatory properties, which can help reduce swelling, redness, and discomfort associated with nail fungus. By soothing inflamed tissues and promoting healing, neem oil provides relief from the symptoms of nail fungus while addressing the root cause of the infection.
The effectiveness of neem oil in treating nail fungus is supported by both anecdotal evidence and scientific studies. Many individuals have reported positive outcomes after using neem oil as a topical treatment for nail fungus, experiencing improvements in nail appearance, texture, and overall nail health.
Incorporating neem oil into a comprehensive nail care routine can offer a natural and holistic approach to managing nail fungus. By harnessing the therapeutic power of neem oil, individuals can promote healthy nail growth, restore the appearance of affected nails, and alleviate the discomfort associated with nail fungus infection.
The Science Behind Neem Oil
Research has shown that neem oil contains compounds like nimbidin and nimbin that exhibit potent antifungal activity. These compounds target the fungal cells, disrupting their growth and ultimately leading to their demise. Additionally, neem oil’s anti-inflammatory properties can help alleviate discomfort associated with nail fungus.
How to Use Neem Oil for Nail Fungus
- Clean and trim the affected nails: Start by washing the affected area with warm water and soap, then trim the nails to remove any excess debris.
- Apply neem oil directly: Using a clean cotton swab or ball, apply a few drops of neem oil directly to the affected nails, ensuring thorough coverage.
- Massage gently: Massage the neem oil into the nails and surrounding skin, allowing it to penetrate deeply.
- Repeat regularly: For optimal results, repeat this process twice daily, preferably in the morning and before bedtime.
Neem Oil Nail Fungus Dosage and Application
When using neem oil for nail fungus treatment, it’s essential to use a sufficient amount to ensure thorough coverage of the affected nails and surrounding skin. Here’s a general guideline on how much neem oil to use:
- Drops: Start by applying a few drops of neem oil directly to the affected nails. The exact number of drops will depend on the size of the affected area and the severity of the fungus. Typically, 2-3 drops per nail should be sufficient to cover the entire nail surface adequately.
- Coverage: Ensure that you cover not only the nails but also the surrounding skin, as fungal infections can spread to adjacent areas if left untreated. Use a clean cotton swab or ball to apply the neem oil, making sure to reach all affected areas.
- Massage: After applying the neem oil, gently massage it into the nails and surrounding skin. This helps the oil penetrate deeper into the nail bed and ensures maximum effectiveness against the fungus. Be gentle to avoid causing any discomfort or irritation to the affected area.
- Frequency: Repeat the application process twice daily for optimal results – once in the morning and once before bedtime. Consistency is key, so make it a part of your daily nail care routine for several weeks to see noticeable improvements in nail health.
If you find that a few drops of neem oil are not providing sufficient coverage or if you have multiple affected nails, you can adjust the amount accordingly. Just ensure that all affected areas receive adequate treatment with neem oil to effectively combat the nail fungus.
Remember to be patient and persistent with neem oil treatment, as it may take time to see significant improvements in nail health.
Neem Oil vs. Other Nail Fungus Treatments:
When considering treatment options for nail fungus, it’s essential to weigh the pros and cons of various alternatives to neem oil. Here’s how neem oil compares to some conventional and alternative treatments:
Oral Antifungal Medications:
Neem Oil: Neem oil is a natural remedy derived from the neem tree, known for its antifungal properties. Unlike oral antifungal medications, which may carry the risk of side effects such as gastrointestinal upset, liver damage, and drug interactions, neem oil is generally well-tolerated and has a lower likelihood of systemic adverse effects. Additionally, neem oil offers a safer alternative for individuals with sensitivities to synthetic drugs or underlying health conditions that preclude the use of oral medications.
Topical Antifungal Treatments (e.g., medicated nail polishes):
Neem Oil: Neem oil’s natural composition enables it to penetrate the nail bed effectively and target the underlying fungal infection. Unlike topical treatments like medicated nail polishes, which may struggle to permeate the thick layers of the nail and reach the site of infection, neem oil delivers its antifungal compounds directly to the affected area, enhancing its efficacy in combating nail fungus from within. Additionally, neem oil’s holistic approach addresses both the symptoms and underlying cause of nail fungus, promoting healthy nail regeneration and supporting the body’s natural defense mechanisms.
Home Remedies (e.g., vinegar soaks, tea tree oil):
Neem Oil: While home remedies like vinegar soaks and tea tree oil are popular options for nail fungus treatment, they may lack the potent antifungal properties and comprehensive approach offered by neem oil. Neem oil’s natural compounds, such as nimbidin and nimbin, exhibit strong inhibitory effects against fungal growth and replication, making it a more effective solution for stubborn nail fungus infections. Additionally, neem oil’s anti-inflammatory properties soothe inflammation and promote healing, providing relief from discomfort and supporting overall nail health.
Professional Treatments (e.g., laser therapy, prescription antifungal creams):
Neem Oil: While professional treatments like laser therapy and prescription antifungal creams may offer faster results for severe nail fungus infections, they often come with higher costs and potential side effects. Neem oil provides a natural and cost-effective alternative that is well-suited for mild to moderate cases of nail fungus. Its gentle yet potent antifungal action, coupled with its minimal side effect profile, makes it a preferred choice for individuals seeking a holistic approach to nail fungus treatment without the need for invasive procedures or prescription medications.
Conclusion
Neem oil holds promise as a natural and effective remedy for nail fungus. Its antifungal properties, coupled with its anti-inflammatory benefits, make it a compelling option for those seeking an alternative to conventional treatments. By understanding how to use neem oil properly and incorporating it into a regular nail care routine, individuals can take proactive steps towards healthier, fungus-free nails.
Why are my toenails brittle? Causes, treatment and nutrition

Brittle toenails can be a source of discomfort and self-consciousness, affecting not only the appearance but also the overall health of your feet. Whether you’re dealing with yellow, thick, dry, splitting, or crumbling nails, understanding the underlying causes and effective treatment options is crucial for regaining confidence in your feet’s appearance and health.
Causes of Brittle Toenails
Brittle toenails can stem from various factors, ranging from medical conditions to lifestyle choices. Understanding the root cause is the first step toward finding an appropriate treatment.
Here are some common reasons why toenails may become brittle, each explained in more detail to provide a deeper understanding for the reader:
- Hypothyroidism: When the thyroid gland doesn’t produce enough hormones, it can lead to brittle nails, among other symptoms like weight gain and fatigue. The thyroid plays a crucial role in regulating metabolism, and its dysfunction can affect various bodily functions, including nail health. Brittle nails in individuals with hypothyroidism often accompany other signs of thyroid dysfunction, making it important to consider this condition as a potential cause.
- Nutritional Deficiencies: Nails require a balanced intake of essential nutrients to stay strong and healthy. Deficiencies in vitamins and minerals, such as biotin, vitamin C, iron, and zinc, can weaken nails and contribute to brittleness. Conditions like bulimia, anorexia, and anemia, which involve inadequate nutrient intake or absorption, can deprive the body of vital nutrients necessary for nail health. Understanding the role of nutrition in maintaining strong nails underscores the importance of a well-rounded diet for overall nail health.
- Overuse of Chemical Products: Excessive exposure to nail polish, polish removers, and cuticle solvents can strip the nails of moisture and essential oils, leading to brittleness. Individuals working in nail salons or frequently changing nail colors may be particularly susceptible to this type of damage. Harsh chemicals can weaken the structure of the nails, making them prone to splitting, peeling, and breakage. Proper protection and moderation in the use of chemical products are essential for preserving nail health.
- Excessive Moisture or Dryness: Paradoxically, both too little and too much moisture can contribute to brittle toenails. Constant exposure to water, as experienced by swimmers, lifeguards, or individuals with occupations involving water immersion, can weaken the nails and make them prone to brittleness. Conversely, frequent exposure to strong soaps or over washing can strip the nails of natural oils, leading to dryness and brittleness. Maintaining a balanced level of moisture through proper hydration and moisturization is key to preventing nail brittleness.
- Aging: As we age, our bodies undergo various changes, including a decreased ability to retain moisture. This natural aging process can affect the health and appearance of the nails, making them dry, brittle, and more susceptible to damage. Understanding the impact of aging on nail health emphasizes the importance of proactive care and maintenance as we grow older.
- Fungal Infections: Toenail fungus, also known as onychomycosis, is a common fungal infection that can affect the health of the nails. Fungal infections weaken the nails, causing them to become discolored, thickened, and brittle. Yellow, thick, and crumbly toenails are common signs of toenail fungus, which can be challenging to treat without proper intervention. Recognizing the symptoms of fungal infections and seeking timely treatment is essential for preventing further damage to the nails.
- Other Medical Conditions: Certain medical conditions, such as Raynaud’s Phenomenon, psoriasis, eczema, and other skin conditions, can impact nail health and contribute to brittleness. These conditions may affect blood flow, skin integrity, or immune function, leading to changes in the nails’ appearance and texture. Understanding the relationship between underlying medical conditions and nail health is crucial for identifying and addressing the root cause of brittle toenails.
Treatment Options
Fortunately, several treatment options are available to address brittle toenails and restore their strength and appearance.
Here are some effective treatments for brittle toenails, presented with the user in mind to ensure clarity and practicality:
- Biotin Supplements: Biotin, a B-complex vitamin, has been found to strengthen weak, brittle nails. Over-the-counter biotin supplements, such as Appearex, can be easily incorporated into your daily routine. Studies suggest that taking a daily dose of 2.5 milligrams of biotin can significantly improve nail strength over time. By adding biotin supplements to your diet, you can support your nails’ health from within and promote stronger, more resilient nails.
- Genadur: For individuals seeking a prescription treatment for brittle nails, Genadur offers a promising solution. Approved by the FDA, Genadur is specifically designed to address fragile, brittle nails. Its once-daily brush-on application makes it convenient to use, with visible results often noticeable within two to three weeks. By following the prescribed regimen, you can enhance the strength and appearance of your toenails and regain confidence in your feet’s health.
- Proper Nail Care: Adopting good hygiene and trimming habits is essential for maintaining overall nail health. Simple practices such as regular moisturizing, foot soaks, and wearing properly fitting shoes can make a significant difference in preventing nail brittleness. By keeping your toenails clean, well-moisturized, and properly trimmed, you can minimize the risk of damage and promote healthy nail growth.
- Address Underlying Health Issues: If your brittle toenails are caused by underlying medical conditions such as hypothyroidism or fungal infections, it’s crucial to address these issues with appropriate medical treatment. Consult with a healthcare professional to identify and treat any underlying health issues contributing to your nail problems. By addressing the root cause, you can effectively manage brittle toenails and prevent recurrence in the future.
- Avoid Harsh Chemicals: Limiting exposure to harsh chemicals is essential for protecting your nails from damage. Avoiding nail polish, polish removers, and other chemical products that can strip the nails of moisture and weaken their structure is important. Instead, opt for gentle, moisturizing nail care products that nourish and protect your nails. By choosing nail products with natural ingredients and avoiding harsh chemicals, you can promote healthier, stronger nails over time.
To strengthen brittle toenails through nutrition, consider incorporating these nutrient-rich foods into your diet:
- Protein-Rich Foods: Nails are made of a protein called keratin, so ensuring an adequate intake of protein is crucial for nail health. Incorporate sources of lean protein such as poultry, fish, eggs, legumes, nuts, and seeds into your meals.
- Biotin: Biotin, also known as vitamin B7, is essential for nail strength and growth. Include biotin-rich foods in your diet such as eggs, nuts (especially almonds and peanuts), seeds (such as sunflower seeds), whole grains, bananas, mushrooms, and avocado.
- Omega-3 Fatty Acids: Omega-3 fatty acids help to moisturize and strengthen nails from within. Add omega-3-rich foods like fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, walnuts, and hemp seeds to your diet.
- Vitamin C: Vitamin C is essential for collagen production, which is important for nail strength and resilience. Incorporate vitamin C-rich foods such as citrus fruits (oranges, lemons, grapefruits), strawberries, kiwi, bell peppers, tomatoes, and broccoli into your meals.
- Iron: Iron deficiency can lead to brittle nails, so ensure you’re getting enough iron from sources such as lean meats, poultry, fish, tofu, beans, lentils, fortified cereals, spinach, and other leafy greens.
- Zinc: Zinc plays a role in nail growth and repair. Include zinc-rich foods like shellfish (oysters, crab, shrimp), lean meats, poultry, nuts, seeds, whole grains, and dairy products in your diet.
- Vitamin E: Vitamin E is an antioxidant that promotes nail health by protecting them from damage. Enjoy foods rich in vitamin E such as almonds, sunflower seeds, spinach, avocado, olive oil, and wheat germ.
Conclusion
Brittle toenails can indeed be frustrating and uncomfortable, but there’s hope for improvement with the right approach to understanding and treatment. By looking into the underlying causes and adopting proper nail care habits, you can take significant steps toward restoring the health and appearance of your nails.
Addressing the root causes of brittle toenails is essential for effective treatment. Whether it’s addressing medical conditions like hypothyroidism or fungal infections or making lifestyle changes to avoid excessive moisture or exposure to harsh chemicals, understanding the underlying factors contributing to your condition is key.
In addition to addressing the root causes, adopting proper nail care habits can greatly contribute to nail health. Simple practices such as regular moisturizing, proper trimming, and avoiding harsh chemicals can make a significant difference in preventing further damage and promoting healthy nail growth.
Considering treatment options like biotin supplements and prescription products like Genadur can also provide targeted support for strengthening and restoring brittle toenails. Biotin supplements have shown promising results in improving nail strength, while prescription products like Genadur offer FDA-approved solutions for fragile nails.
If you’re unsure about the best treatment approach for your specific condition, don’t hesitate to consult with a healthcare professional. They can provide personalized guidance and recommendations tailored to your individual needs, ensuring that you receive the most effective treatment for your brittle toenails.
With the right understanding, treatment approach, and professional guidance, you can regain confidence in your feet and enjoy healthy, resilient toenails once again. Don’t let brittle toenails hold you back—take proactive steps toward nail health and reclaim your confidence today.
Toenail Fungus How to Treat Infection
The most common treatment for toenail fungus is typically oral antifungal medication, such as terbinafine (Lamisil) or itraconazole (Sporanox). These medications work systemically to target the fungal infection throughout the body, including in the nails. They are often prescribed for several weeks or months, depending on the severity of the infection.
Comprehensive Guide: How to Treat Toenail Fungus Effectively
Toenail fungus, medically known as onychomycosis, is a common condition that affects many individuals worldwide. Characterized by white, brown, or yellow spots on the toenails, toenail fungus can lead to thickened nails and discomfort if left untreated. This comprehensive guide aims to provide detailed insights into toenail fungus how to treat effectively, covering prescription treatments, home remedies, prevention strategies, and essential tips for managing the condition.
Understanding “The Toenail Fungus”
Toenail fungus, also known as onychomycosis, is a common condition caused by fungal growth on the toenails. Imagine your toenails as tiny gardens where fungi love to grow, especially in warm and moist environments like pool decks, locker rooms, or inside sweaty shoes. These places provide the perfect conditions for fungi to thrive and multiply.
While toenail fungus itself isn’t usually life-threatening, ignoring it can lead to worsening symptoms over time. If left untreated, toenail fungus can cause discomfort and pain, making it difficult to walk or wear shoes comfortably. Moreover, the fungus can spread from one toenail to another, affecting multiple nails and increasing the severity of the infection. In some cases, untreated toenail fungus can even lead to secondary infections, making the situation more complicated and uncomfortable.
So, it’s essential to pay attention to any changes in your toenails and take action if you notice signs of toenail fungus. Early intervention can prevent the condition from worsening and help you avoid potential complications down the road. When considering toenail fungus how to treat, immediate attention and proper care are crucial to effectively managing this pesky problem.
Toenail Fugus Diagnosis and Evaluation
When you suspect you have toenail fungus, getting a proper diagnosis is crucial for effective treatment. Typically, diagnosing toenail fungus requires a visit to a healthcare provider, who will conduct a thorough examination of your toenails. During this examination, your healthcare provider will closely inspect the affected nails, looking for characteristic signs of toenail fungus such as discoloration, thickening, or crumbling.
In some cases, your healthcare provider may need to take nail clippings or scrapings from the affected nails for further analysis. These samples are then sent to a laboratory for testing to confirm the presence of fungal infection. This step is essential because other conditions, such as psoriasis, can mimic the symptoms of toenail fungus. By accurately diagnosing the condition, your healthcare provider can determine the most suitable treatment approach tailored to your specific needs. When it comes to toenail fungus how to treat, a precise diagnosis lays the foundation for effective management.
To diagnose toenail fungus, a healthcare provider will:
- Conduct a thorough examination of the affected toenails.
- Look for signs such as discoloration, thickening, or crumbling.
- Collect nail clippings or scrapings for laboratory analysis if needed.
Laboratory testing helps differentiate toenail fungus from conditions like psoriasis.
Accurate diagnosis guides the selection of the most suitable treatment approach.
So, if you suspect you have toenail fungus, don’t hesitate to seek medical attention. A healthcare provider can provide an accurate diagnosis and recommend the appropriate treatment to help you manage the condition effectively.
Nail Fungus Prescription Treatments
When it comes to treating toenail fungus, prescription medications offer several options to effectively combat the infection. These medications come in various forms, including creams, sprays, gels, and oral medications, each with its own benefits and considerations.
1. Topical Treatments:
- Creams, sprays, and gels like ciclopirox, efinaconazole, and tavaborole are commonly prescribed for surface fungus. These medications work by directly targeting the fungal infection on the surface of the toenail.
- While these topical treatments can be effective, they often require consistent and prolonged daily use to achieve visible results. It’s essential to follow your healthcare provider’s instructions carefully and continue treatment as directed.
2. Oral Antifungal Drugs:
- For more severe cases of toenail fungus or infections that have penetrated deeper into the nail bed, oral antifungal drugs may be recommended.
- Drugs like itraconazole and terbinafine are commonly prescribed oral medications that offer higher success rates in treating toenail fungus. These medications work systemically, reaching the site of infection through the bloodstream.
- However, oral antifungal drugs may pose risks of side effects and require close monitoring by healthcare providers. Common side effects may include gastrointestinal issues, headaches, and liver abnormalities. Patients with certain medical conditions or taking specific medications may need special consideration when using oral antifungal drugs.
Prescription treatments for toenail fungus provide effective options for combating the infection and promoting nail health. Whether you go for topical treatments or oral medications, it’s essential to discuss the benefits and risks with your healthcare provider to determine the most suitable treatment approach for your individual needs, especially in the context of toenail fungus how to treat. Additionally, adherence to treatment guidelines and regular monitoring can help maximize the effectiveness of prescription medications while minimizing potential side effects
Nail Removal & Safety Precautions
When toenail fungus becomes severe and deeply entrenched, nail removal may be considered as a treatment option to effectively eliminate the infection and prevent its recurrence, which is crucial in understanding toenail fungus how to treat. In such cases, healthcare providers may recommend either nonsurgical or surgical methods, depending on the severity of the infection and the patient’s individual circumstances.
Nonsurgical Methods:
- Nonsurgical approaches involve the application of urea ointment to soften the nail bed, facilitating the removal of the affected nail material. Urea works by breaking down the protein structure of the nail, making it easier to trim or remove the infected portions.
- This method is often preferred for less severe cases of toenail fungus or for individuals who prefer noninvasive treatment options. It aims to promote healthy nail regrowth by removing the diseased nail material and allowing the nail bed to heal properly.
Surgical Procedures:
- In more severe cases where the toenail fungus is deeply embedded and causing significant discomfort or complications, surgical nail removal may be necessary.
- Surgical procedures for toenail removal typically involve either partial or complete removal of the affected nail under local anesthesia. The surgeon may use specialized tools to carefully lift and remove the nail, ensuring that the nail bed is adequately cleaned and treated.
- The goal of surgical nail removal is to eliminate the source of the fungal infection and promote the growth of a healthy nail. After the procedure, patients may be advised to apply topical antifungal medications to prevent recurrence and facilitate nail regrowth.
Both nonsurgical and surgical methods aim to address the underlying fungal infection while promoting the regeneration of a healthy nail. However, the choice between these approaches depends on factors such as the severity of the infection, patient preferences, and the recommendations of the healthcare provider. Regardless of the method chosen, close follow-up care and adherence to post-treatment instructions are essential for achieving optimal outcomes and preventing future infections.
It’s important to note that removing toenails at home can carry risks of infection and complications, here’s a step-by-step guide for safely removing a toenail at home if advised by a healthcare professional:
1. Gather Supplies:
- Sterile nail clippers or scissors
- Sterile gauze pads
- Antiseptic solution (e.g., hydrogen peroxide or rubbing alcohol)
- Antibiotic ointment
- Bandages or adhesive bandages
2. Prepare the Area:
- Wash your hands thoroughly with soap and water.
- Clean the affected toe and surrounding area with warm water and mild soap.
- Use an antiseptic solution to clean the toenail and the tools you will be using to remove it.
3. Softening the Nail:
- Soak your foot in warm, soapy water for about 10-15 minutes to soften the nail and make it easier to trim.
4. Trimming the Nail:
- Carefully trim the affected nail using sterile nail clippers or scissors. Trim the nail straight across, avoiding cutting it too short or into the surrounding skin.
- If the nail is thick or hard to trim, gently file the surface of the nail to thin it out before attempting to trim it.
5. Removing the Affected Portion:
- If only a portion of the nail is affected, focus on removing the damaged or infected area. Trim the nail back to the healthy nail bed, ensuring that all visible signs of infection are removed.
- Take care to avoid causing pain or injury to the surrounding skin.
6. Cleaning and Dressing:
- After removing the affected portion of the nail, clean the area with an antiseptic solution to reduce the risk of infection.
- Apply a small amount of antibiotic ointment to the nail bed to promote healing and prevent infection.
- Cover the area with a sterile gauze pad and secure it in place with a bandage or adhesive bandage.
7. Monitoring and Care:
- Keep the area clean and dry, changing the dressing regularly to prevent infection.
- Monitor the site for signs of infection, such as increased redness, swelling, pain, or drainage.
- Follow any additional instructions provided by your healthcare provider for post-removal care and follow-up appointments.
Over-the-Counter Nail Fungus Treatments
For individuals with mild cases of toenail fungus, over the counter (OTC) treatments offer accessible options for managing the infection. These OTC treatments typically come in the form of antifungal creams, gels, sprays, and patches, providing convenience and ease of use. However, it’s essential to understand the limitations of these products, especially when dealing with moderate to severe infections.
OTC Antifungal Products:
- Antifungal creams, gels, sprays, and patches contain active ingredients designed to combat fungal growth on the toenails. Common antifungal agents found in OTC products include clotrimazole, terbinafine, and undecylenic acid.
- These OTC treatments are suitable for mild cases of toenail fungus and may provide symptomatic relief by reducing itching, inflammation, and fungal proliferation.
- However, OTC antifungal products are generally less effective for moderate to severe infections that have penetrated deeper into the nail bed. In such cases, adjunct therapy with prescription medications may be necessary to achieve optimal outcomes.
Adjunct Therapy:
- In cases where OTC treatments alone are insufficient to manage the toenail fungus effectively, healthcare providers may recommend adjunct therapy with prescription medications.
- Prescription antifungal drugs, such as oral medications or medicated nail polishes, offer higher efficacy in treating moderate to severe toenail fungus by targeting the infection systemically or directly at the site of the nail bed.
- Combining OTC treatments with prescription medications can enhance the overall effectiveness of treatment and improve outcomes for individuals with more severe infections.
OTC treatments play a valuable role in managing mild cases of toenail fungus and providing symptomatic relief; however, it’s essential to recognize their limitations in treating moderate to severe infections, a critical aspect of understanding toenail fungus how to treat. If you suspect you have toenail fungus or have concerns about the effectiveness of OTC treatments, consulting with a healthcare provider is recommended. A healthcare provider can assess the severity of the infection and recommend appropriate treatment options tailored to your individual needs.
Alternative At Home Remedies for Toenail Fungus
In addition to conventional treatments, various alternative remedies have been explored for the treatment of toenail fungus. These alternative therapies, including tea tree oil, Vicks VapoRub, apple cider vinegar, and baking soda, have gained attention for their potential antifungal properties. However, it’s important to approach these remedies with caution and understanding of their current scientific evidence.
Tea Tree Oil:
- Tea tree oil, derived from the leaves of the tea tree (Melaleuca alternifolia), has been studied for its antifungal properties. Some research suggests that tea tree oil may be effective in combating toenail fungus when applied topically.
- While initial studies show promising results, more research is needed to establish the efficacy and safety of tea tree oil for treating toenail fungus. It’s advisable to use tea tree oil cautiously and consult a healthcare provider before incorporating it into your treatment regimen.
Vicks VapoRub:
- Vicks VapoRub, a topical ointment commonly used to relieve cough symptoms, contains ingredients like camphor, eucalyptus oil, and menthol, which have been suggested to have antifungal properties.
- Limited studies have explored the use of Vicks VapoRub for toenail fungus, with some indicating potential benefits. However, more research is needed to validate its effectiveness and safety for this purpose.
Apple Cider Vinegar:
- Apple cider vinegar, a popular home remedy known for its antimicrobial properties, has been advocated for treating toenail fungus. It is often used in foot soaks or applied directly to the affected nails.
- While anecdotal evidence suggests that apple cider vinegar may help inhibit fungal growth, scientific studies supporting its efficacy in treating toenail fungus are lacking. Further research is necessary to determine its effectiveness and optimal use.
Baking Soda:
- Baking soda, or sodium bicarbonate, has been investigated for its potential antifungal properties. Some studies suggest that baking soda may help inhibit fungal growth and reduce symptoms of toenail fungus when applied topically or used in foot soaks.
- Despite these findings, more rigorous research is needed to confirm the efficacy of baking soda for treating toenail fungus and to establish the optimal methods of application.
While alternative remedies like tea tree oil, Vicks VapoRub, apple cider vinegar, and baking soda may hold promise for treating toenail fungus, their effectiveness and safety require further investigation. It’s advisable to approach these remedies cautiously and consult a healthcare provider before using them as part of your treatment plan.
Prevention Strategies for Toenail Fungus
Preventing toenail fungus is crucial for maintaining optimal foot health and reducing the risk of developing fungal infections. Incorporating simple yet effective preventive measures into your daily routine can help minimize the likelihood of toenail fungus. Here are some key strategies for preventing toenail fungus:
Practice Good Foot Hygiene:
- Keep your feet clean and dry by washing them regularly with soap and water. Pay special attention to the areas between your toes, where moisture can accumulate.
- After washing, thoroughly dry your feet, including the spaces between your toes, to prevent moisture buildup, which creates an ideal environment for fungal growth.
Wear Breathable Footwear:
- Choose shoes made from breathable materials, such as leather or mesh, that allow air circulation around your feet. Avoid wearing tight-fitting shoes or synthetic materials that can trap moisture.
- Consider wearing moisture-wicking socks to help keep your feet dry, especially during physical activity or in warm weather.
Avoid Barefoot Walking in Communal Areas:
- Refrain from walking barefoot in communal areas like locker rooms, public showers, swimming pools, and gyms, where fungal infections can easily spread.
- Wear flip-flops or shower shoes when using public facilities to minimize direct contact with potentially contaminated surfaces.
Regularly Change Socks and Shoes:
- Change your socks daily, particularly if your feet tend to sweat excessively. Moisture-wicking socks can help absorb sweat and keep your feet dry.
- Rotate your shoes to allow them to air out between wearings. Avoid wearing the same pair of shoes every day, as this can contribute to moisture buildup and fungal growth.
Keep Nails Trimmed:
- Trim your toenails regularly, cutting them straight across and avoiding rounded edges. Shorter nails are less prone to trauma and less likely to harbor fungi.
- Use clean, properly sanitized nail clippers to avoid introducing bacteria or fungi into the nail bed during trimming.
Avoid Nail Injuries:
- Take precautions to prevent nail injuries, such as avoiding activities that may cause trauma to the toenails, like kicking or stubbing your toes.
- Wear protective footwear, such as steel-toed shoes, when engaging in activities that pose a risk of nail injury, such as construction work or sports.
Incorporating these preventive measures into your daily routine, you can help protect your toenails from fungal infections and maintain overall foot health. If you notice any signs of toenail fungus or have concerns about your foot hygiene practices, consult a healthcare provider for guidance and appropriate treatment options.
FAQ Section: Toenail Fungus Treatment
1. What is the fastest way to cure toenail fungus?
- While there is no instant cure for toenail fungus, oral antifungal medications like terbinafine and itraconazole are often considered the fastest treatment options. These medications work systemically to target the fungal infection, but results may still take several weeks or months to become visible.
2. Can you remove fungus toenail at home?
- While it is possible to attempt to remove a fungus-infected toenail at home, it is not recommended without proper guidance from a healthcare professional. Home removal methods may not effectively eliminate the underlying fungal infection and can increase the risk of injury or secondary infections.
3. What is the most successful treatment for toenail fungus?
- The most successful treatment for toenail fungus varies depending on the severity of the infection and individual factors. Oral antifungal medications, such as terbinafine and itraconazole, are often considered highly effective, particularly for moderate to severe cases of toenail fungus.
4. What is the best treatment for fungal toenails?
- The best treatment for fungal toenails depends on various factors, including the extent of the infection, medical history, and treatment preferences. Prescription antifungal medications, topical treatments, laser therapy, and surgical interventions are among the options available. Consulting with a healthcare provider can help determine the most suitable treatment approach for your specific case.
5. What is the sock trick for toenail fungus?
- The “sock trick” involves applying an antifungal cream or ointment to the affected toenail(s) and covering them with clean socks overnight. This method helps enhance the penetration of the antifungal medication into the nail bed and creates a conducive environment for treatment while you sleep.
6. What worsens toenail fungus?
- Several factors can exacerbate toenail fungus, including prolonged exposure to warm, moist environments (such as sweaty shoes or wet socks), poor foot hygiene, compromised immune function, wearing tight-fitting footwear, and untreated fungal skin infections (such as athlete’s foot).
7. Is hydrogen peroxide good for toenail fungus?
- While hydrogen peroxide may have some antifungal properties, there is limited scientific evidence supporting its efficacy in treating toenail fungus. Additionally, hydrogen peroxide can cause skin irritation and may not effectively penetrate the nail bed to target the underlying infection.
8. Is it OK to cut toenail fungus?
- It is generally safe to trim toenails affected by fungus, but caution should be exercised to avoid causing further injury or spreading the infection. Use clean, sterilized nail clippers and avoid cutting the nails too short or aggressively, as this can worsen the condition.
9. Why does Vicks VapoRub work on nail fungus?
- Vicks VapoRub contains ingredients like camphor, eucalyptus oil, and menthol, which have potential antifungal properties. While some individuals report success with Vicks VapoRub for toenail fungus, scientific evidence supporting its effectiveness is limited, and more research is needed to understand its mechanisms of action.
10. Do I need to throw away my shoes if I have toenail fungus?
- While it’s not always necessary to discard shoes if you have toenail fungus, it’s essential to practice proper foot hygiene and disinfect your footwear regularly. Consider using antifungal sprays or powders inside your shoes and rotating between different pairs to allow them to dry thoroughly between wearing.
11. What happens if you have toenail fungus for too long?
- If left untreated, toenail fungus can worsen over time, leading to thickened, discolored nails, pain, discomfort, and an increased risk of complications. In severe cases, the infection may spread to other nails or surrounding skin, causing secondary infections or chronic nail deformities.
12. What household item kills toenail fungus?
- Several household items, such as vinegar, baking soda, and tea tree oil, have been explored for their potential antifungal properties. While these remedies may offer some benefit, their effectiveness in treating toenail fungus varies, and more research is needed to validate their use as standalone treatments. It’s advisable to consult a healthcare provider before relying solely on household items for toenail fungus treatment.
Summary
To treat toenail fungus effectively, it’s essential to adopt a multifaceted approach. This involves medical treatments prescribed by a healthcare provider, such as oral or topical antifungal medications. Additionally, home remedies like tea tree oil or apple cider vinegar soaks can provide supplementary relief. Preventive measures, including practicing good foot hygiene and wearing breathable footwear, are crucial for reducing the risk of recurrence. Consulting a healthcare provider for personalized treatment recommendations and regular follow-up appointments are key steps in managing toenail fungus and maintaining overall foot health.
References:
Ferrari, J. (2014). Fungal toenail infections. BMJ Clinical Evidence, 2014(13), 1715 Nenoff, P., et al. (2023). S1 Guideline onychomycosis. J Dtsch Dermatol Ges, 21(6), 678–692
Wide Calf Comfort: Compression Socks Large Calves

3 x CopperZen Wide Calf Compression Socks – (L/XL)

Choose your size:
How To Order Compression Socks for Large Calves
Step 1: Click Here to Order Your Compression socks
Compression socks are specially designed garments that provide graduated pressure to the legs, promoting better circulation and reducing swelling and fatigue. While they offer a myriad of benefits for various individuals, those with larger calves often struggle to find socks that fit properly. This is where compression socks tailored for larger calves come in, offering a snug yet comfortable fit without sacrificing effectiveness.
Step 2: Click the Order Now Button
The Benefits of Compression Socks for Large Calves
- Improved Circulation: One of the primary benefits of compression socks is their ability to enhance blood flow in the legs. By exerting gentle pressure on the veins, they help push blood back towards the heart, reducing the risk of swelling and blood clots.
- Reduced Swelling and Fatigue: If you spend long hours on your feet or have a job that requires prolonged sitting, you may experience swelling and fatigue in your legs. Compression socks can help alleviate these symptoms by providing support and preventing fluid buildup in the lower extremities.
- Enhanced Comfort: Finding socks that fit comfortably over large calves can be a challenge. Compression socks for large calves are designed with stretchy, breathable materials that conform to your legs without feeling restrictive, ensuring all-day comfort and support.
- Prevention of Varicose Veins: Varicose veins are a common issue for individuals with poor circulation or a family history of vein problems. Wearing compression socks can help prevent the development of varicose veins by improving blood flow and reducing pressure on the veins.
- Faster Muscle Recovery: Whether you’re an athlete or simply enjoy staying active, compression socks can aid in muscle recovery by increasing oxygen delivery to the muscles and flushing out lactic acid buildup. This can help reduce soreness and stiffness after intense workouts or physical activity.
- Temperature Regulation: Compression socks are made from moisture-wicking fabrics that help regulate temperature and keep your legs dry and comfortable throughout the day. Whether it’s hot or cold outside, compression socks provide the perfect balance of warmth and breathability.
Step 3: Choose 1 Pair, 3 Pairs or 5 Pairs
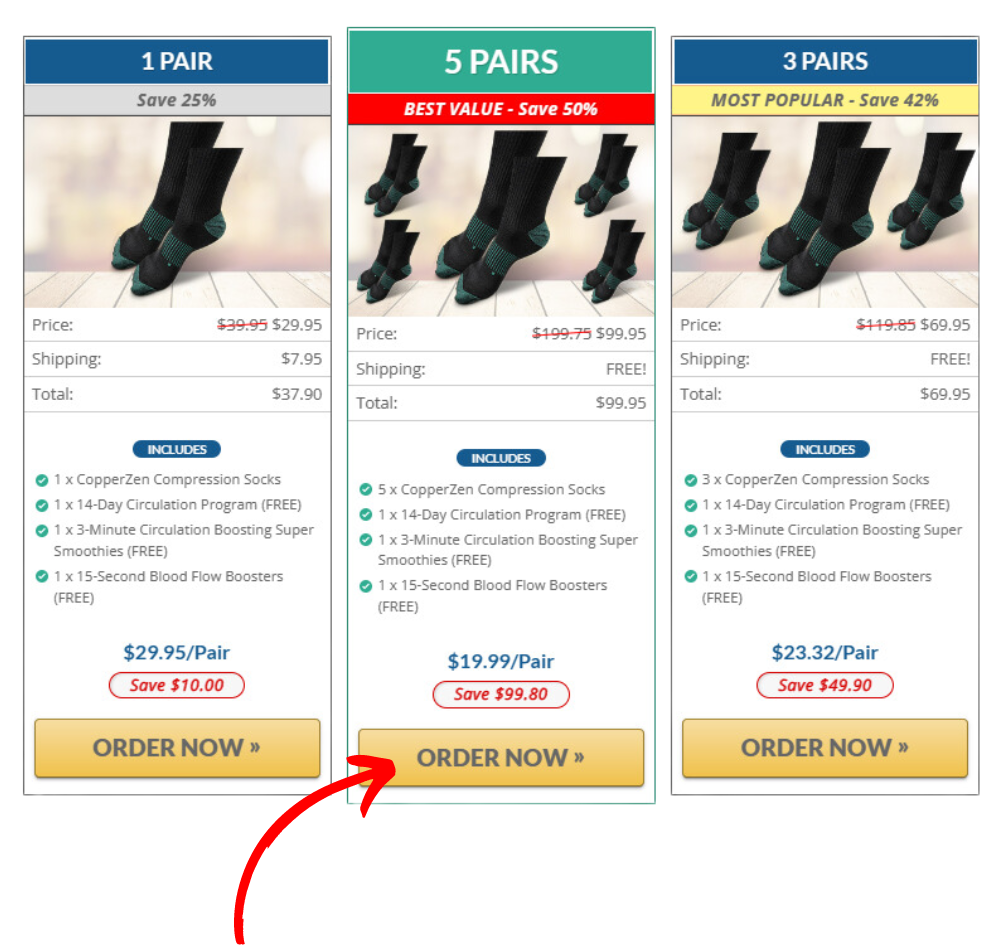
Compression socks promote good circulation through the application of graduated pressure along the legs. This pressure is highest at the ankles and gradually decreases as it moves upward toward the calf and thigh. By compressing the veins and muscles in the lower legs, compression socks help to improve blood flow back to the heart, thus preventing blood from pooling or stagnating in the lower extremities.
As a result, compression socks effectively counteract the effects of gravity, which can cause blood to accumulate in the veins of the legs, leading to swelling, discomfort, and fatigue. By facilitating the return of blood to the heart, compression socks reduce the risk of venous insufficiency, varicose veins, and other circulatory issues. Additionally, improved circulation means that muscles receive a steady supply of oxygen and nutrients, promoting faster recovery and reducing the risk of cramps and muscle fatigue.
Step 4: Choose Your Size
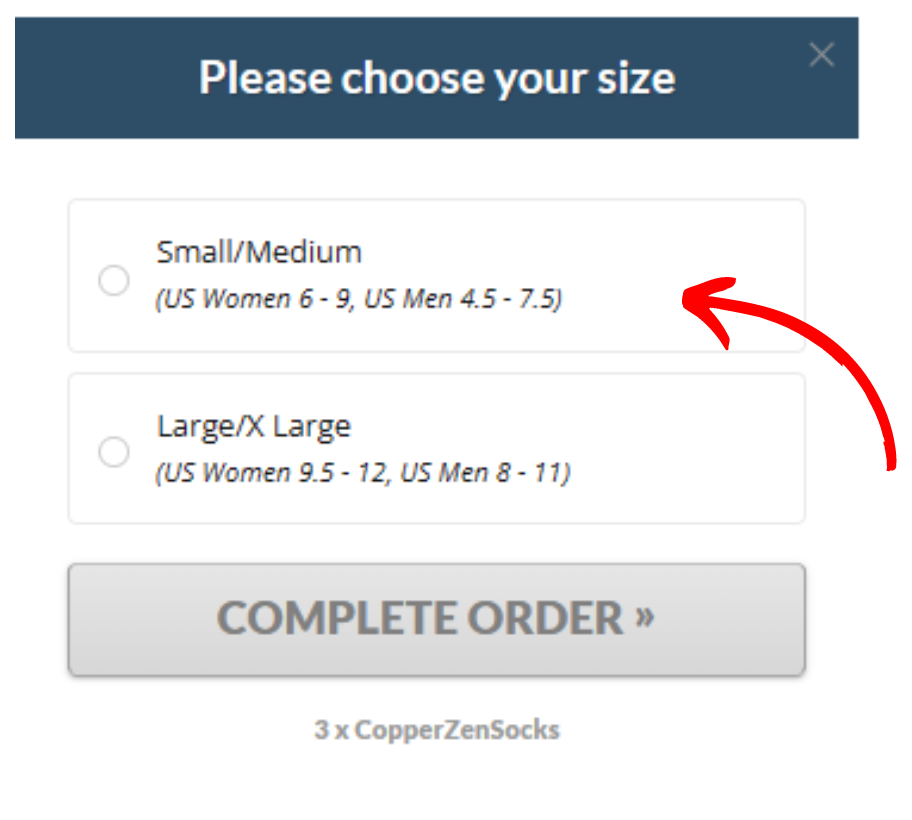
Compression socks for large calves offer a host of benefits for individuals seeking relief from leg discomfort and swelling. By improving circulation, reducing fatigue, and enhancing overall comfort, these specialized socks can make a significant difference in your daily life. Say goodbye to discomfort and hello to a new level of wellness with compression socks designed for your unique needs.
>>Don’t Wait – Improve Your Poor Circulation, Order Now!<<
How To Get Rid of Green Nail Fungus?

Experiencing the unsettling sight of green nails can be concerning, but understanding the causes and treatment options can help ease worries. Green nail syndrome, also known as chloronychia, is a common nail infection characterized by a greenish discoloration of the nails. This comprehensive guide will explore the causes, symptoms, diagnosis, and treatment options for green nail syndrome.
What is Green Nail Syndrome?
Green nail syndrome (GNS), or chloronychia, is a nail infection caused by the bacterium Pseudomonas aeruginosa. This bacterium thrives in moist environments and produces distinctive green pigments, leading to the characteristic discoloration of the nails. GNS can affect both fingernails and toenails and is often associated with onycholysis, where the nail becomes separated from the nail bed.
Causes and Risk Factors
Several factors contribute to the development of green nail syndrome (GNS), making it important to understand the various triggers behind this condition:
Onycholysis
- Onycholysis refers to the separation of the nail from the nail bed, creating a space underneath the nail. This separation provides an ideal environment for bacteria like Pseudomonas aeruginosa to thrive, leading to the characteristic greenish discoloration associated with GNS. Activities or occupations that involve repeated trauma to the nails, such as gardening, cleaning, or plumbing, increase the risk of onycholysis and subsequent GNS.
Damp Environments
- Pseudomonas aeruginosa, the bacteria responsible for GNS, thrives in moist environments. Exposure to water for prolonged periods, such as frequent handwashing, dishwashing, or prolonged immersion in water during activities like swimming or bathing, can create an environment conducive to bacterial growth. Individuals who work in environments with high humidity levels or have occupations that involve frequent contact with water are at increased risk of developing GNS.
Tight-Fitting Shoes
- Wearing tight-fitting shoes can contribute to nail trauma and increase the risk of onycholysis, especially in the toes. Continuous pressure on the toenails from tight shoes can cause damage to the nail plate and surrounding tissue, creating an entry point for bacteria. Activities that require wearing tight shoes for extended periods, such as athletics or certain occupations, may increase the likelihood of developing GNS.
Other Risk Factors
- Certain underlying conditions or habits may predispose individuals to GNS. For example, individuals with nail psoriasis or fungal nail infections may have compromised nail health, making them more susceptible to bacterial infections like GNS. Additionally, habits such as nail biting or picking can cause trauma to the nails, increasing the risk of onycholysis and bacterial colonization.
Symptoms and Diagnosis
The main symptom of green nail syndrome (GNS) is the noticeable greenish discoloration of the nails, ranging from shades of blue-green to dark green or bluish grey. While the discoloration is prominent, individuals may not always experience pain directly in the affected nails. However, the skin surrounding the affected nail, including the cuticle area, may exhibit signs of inflammation such as swelling, tenderness, or redness.
Diagnosing GNS is typically straightforward and primarily based on the clinical appearance of the affected nails. A healthcare professional, often a dermatologist, can readily identify the characteristic green discoloration associated with GNS during a physical examination. In some cases where there is uncertainty about the diagnosis or if additional confirmation is needed, a nail sample may be taken for culture. This involves collecting a small sample of tissue from the affected nail to identify the specific bacteria responsible for the infection.
It’s essential for individuals experiencing symptoms of GNS to seek medical evaluation and diagnosis to ensure appropriate treatment and management. Early detection and intervention can help prevent complications and facilitate prompt resolution of the infection.
Treatment Options
When dealing with green nail fungus, taking proactive steps can help alleviate symptoms and promote healing.
Here’s a detailed guide on how to get rid of green nail fungus:
Trimming the Affected Nail:
- Start by carefully trimming the affected nail to remove any detached or loose portions. This helps eliminate areas where bacteria can thrive and spread.
Keeping the Nails Dry:
- Moisture provides an ideal environment for bacterial growth, so it’s crucial to keep the affected nails as dry as possible. Avoid prolonged exposure to water and moisture, and ensure thorough drying after washing.
Topical Antibiotics:
- Applying topical antibiotics directly to the affected nails can be highly effective in treating green nail fungus. Antibiotics such as bacitracin or polymyxin B are commonly used and can help eliminate the infection when applied consistently two to four times a day.
Home Remedies:
- Home remedies can also play a role in combating green nail fungus. Diluted chlorine bleach or vinegar can be applied topically to suppress bacterial growth and promote healing. Mix chlorine bleach or vinegar with water in a ratio of 1:4 and apply it directly to the affected nails using a cotton ball or swab.
Oral Antibiotics:
- In more severe cases of green nail fungus, oral antibiotics may be necessary to eradicate the infection. Your healthcare provider may prescribe antibiotics such as ciprofloxacin to address the underlying bacterial overgrowth. Follow your doctor’s instructions carefully when taking oral antibiotics and complete the full course of treatment as prescribed.
By incorporating these strategies into your nail care routine, you can effectively manage and eliminate green nail fungus. Consistency and diligence are key, so be sure to adhere to your treatment plan
FAQ:
Q: How to get rid of green nail fungus fast?
A: Trim the affected nail, keep it dry, and apply topical antibiotics regularly.
Q: How to get rid of green nail fungus at home?
A: Keep the affected nail dry and apply topical antibiotics or use diluted chlorine bleach or vinegar.
Q: How to get rid of green nail fungus naturally?
A: Use natural remedies like vinegar or diluted chlorine bleach to suppress bacterial growth.
Q: How to get rid of green toenail fungus?
A: Treat green toenail fungus by keeping the affected nail dry and applying topical antibiotics or natural remedies.
Q: First stage early stage fingernail fungus from acrylic nails
A: Treat early-stage fungal infections resulting from acrylic nails by keeping the affected nail clean, dry, and applying topical antifungal agents as needed.
Conclusion
In conclusion, gaining a comprehensive understanding of green nail syndrome (GNS) and its available treatment options is key to addressing concerns and effectively managing the condition. Whether going for professional treatment or exploring home remedies, taking proactive steps to tackle GNS can lead to healthier nails and provide peace of mind. If you suspect you may have green nail syndrome, don’t hesitate to consult a healthcare professional for personalized advice and guidance on the best course of action tailored to your needs. Your journey to healthier nails begins with seeking the support and expertise you deserve.
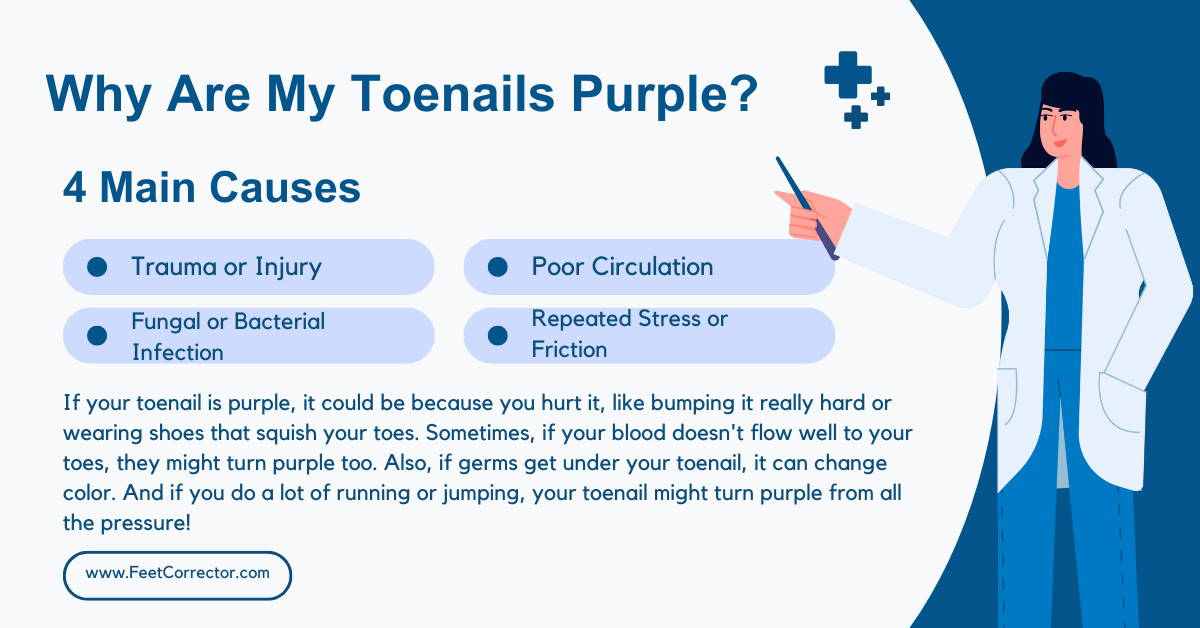
Why Are My Toenails Purple?

Experiencing the shock of purple toenails can often spark curiosity and concern. If you’ve noticed your toenails turning purple underneath, at the cuticle, or appearing light purple, you’re likely seeking answers. This comprehensive guide aims to simplify purple toenails, outlining their various causes, diagnosis methods, treatments, and preventive measures.
Causes of Purple Toenails
Purple toenails can indicate underlying issues that range from benign to potentially serious. Understanding the root causes is crucial for proper management.
Here’s a detailed look at some common triggers:
Footwear-Related Causes
- The type of shoes you wear plays a significant role in toenail health. Tight or ill-fitting shoes can exert pressure on the toes, leading to bruising or injury that manifests as purple toenails. If your toenails are purple at the cuticle, it could be a sign of constant friction or trauma from improperly fitting footwear. Additionally, shoes with narrow toe boxes, such as high heels or pointed shoes, can compress the toes, causing discomfort and potential toenail damage.
Aging and Circulation
- As we age, changes in blood circulation can affect toenail color. Diminished blood flow to the extremities may result in purple or blue toenails. The aging process can lead to reduced elasticity in blood vessels, impairing circulation to the toes. If your toenails appear light purple, it could indicate oxygen deprivation in the nail bed due to poor circulation. Moreover, age-related health conditions such as peripheral artery disease (PAD) can further compromise blood flow to the feet, contributing to toenail discoloration.
Medical Conditions
- Underlying medical conditions can contribute to purple toenails. Diabetes, for instance, can impact blood circulation, particularly in the lower extremities. Persistent high blood sugar levels can damage blood vessels and nerves, leading to reduced blood flow to the toes and subsequent toenail discoloration. Additionally, vascular issues such as peripheral vascular disease (PVD) or venous insufficiency can impair blood flow, resulting in purple toenails. Furthermore, conditions like Raynaud’s disease, characterized by exaggerated vasoconstriction in response to cold or stress, can cause temporary discoloration and coldness in the toes.
Exercise-Related Factors
- Purple toenails are commonly associated with high-impact activities such as running or hiking. Repetitive stress and trauma from these activities can lead to microtrauma in the toenails, resulting in discoloration. If you’re wondering why your toenails are purple and cold after exercise, it could be due to reduced blood flow during intense physical activity. The combination of increased demand for oxygen and vasoconstriction
Diagnosis of Purple Toenails
Determining the underlying cause of purple toenails often requires a thorough examination by a healthcare professional. If you’re experiencing persistent discoloration or other concerning symptoms, it’s advisable to seek medical attention promptly.
What to Expect:
Medical History:
During your appointment, your healthcare provider will likely begin by asking about your medical history, including any pre-existing conditions, medications you’re taking, and any recent changes in your health.
Physical Examination:
Your doctor will conduct a physical examination of your feet and toenails to assess the extent of discoloration and look for any signs of injury, infection, or circulation issues. They may gently press on the toenails to check for tenderness or discomfort.
Diagnostic Tests:
Depending on the findings of the physical examination and your medical history, your doctor may recommend additional diagnostic tests to determine the underlying cause of the purple toenails. These tests may include:
- Nail Scrapings: Your doctor may collect a small sample of tissue from the affected toenail for laboratory analysis. This can help identify any fungal or bacterial infections that may be contributing to the discoloration.
- Blood Tests: Blood tests may be conducted to assess your overall health and check for underlying conditions such as diabetes, peripheral artery disease (PAD), or other circulatory issues that could be affecting blood flow to the toes.
- Imaging Studies: In some cases, your doctor may order imaging studies such as X-rays or ultrasound scans to evaluate the underlying structures of the foot and identify any abnormalities that may be contributing to the purple toenails.
Questions to Ask Your Healthcare Provider:
1. What Could Be Causing My Purple Toenails?
Understanding the potential underlying causes of purple toenails can help you make informed decisions about your treatment plan and preventive measures.
2. What Diagnostic Tests Will You Perform?
Asking about the specific tests your doctor plans to conduct can help you understand the diagnostic process and what to expect during your appointment.
3. Are There Any Treatment Options Available?
Inquiring about available treatment options can help you explore potential solutions for managing your purple toenails and alleviating any associated symptoms.
4. What Can I Do to Prevent Recurrence?
Seeking guidance on preventive measures can help you minimize the risk of future episodes of purple toenails and promote long-term foot health.
5. When Should I Follow Up?
Establishing a follow-up plan with your healthcare provider can ensure that your progress is monitored and any necessary adjustments to your treatment plan are made.
Treatment Options
Treatment for purple toenails depends on the underlying cause. While consulting a healthcare professional is advisable for persistent or severe cases, there are several home remedies and self-care measures you can try:
1. Rest and Elevation
If your purple toenails are due to minor trauma or bruising, the first step is to rest and elevate the affected foot. Elevating your foot above heart level can help reduce swelling and alleviate discomfort.
2. Cold Compress
Applying a cold compress to the area can help reduce inflammation and numb pain. Wrap a few ice cubes in a towel and apply it to the purple toenail for 10-15 minutes several times a day.
3. Over-the-Counter Pain Relievers
Non-prescription pain relievers such as ibuprofen or acetaminophen can help alleviate pain associated with purple toenails. Follow the recommended dosage instructions and consult your doctor if you have any underlying medical conditions or are taking other medications.
4. Foot Soaks
Soaking your feet in warm water can help promote circulation and soothe discomfort. Add Epsom salts or a few drops of essential oils like lavender or tea tree oil to enhance the therapeutic effect. Soak your feet for 15-20 minutes, then pat them dry and apply moisturizer.
5. Proper Foot Hygiene
Keeping your feet clean and dry is essential for preventing infections and promoting healing. Wash your feet daily with mild soap and warm water, paying attention to the area around the toenails. Dry your feet thoroughly, especially between the toes, to prevent fungal growth.
6. Nail Trimming
Trim your toenails straight across to prevent ingrown toenails, which can exacerbate purple toenail symptoms. Use proper nail clippers and avoid cutting the nails too short to reduce the risk of injury.
7. Protective Measures
If your purple toenails are caused by repeated trauma during physical activity, consider protective measures such as wearing cushioned socks and properly fitting shoes. Choose shoes with ample toe room and good arch support to minimize pressure on the toenails.
8. Moisturization
Apply a moisturizing cream or lotion to your feet regularly to keep the skin hydrated and prevent dryness and cracking. Focus on massaging the cream into the toenails and surrounding skin to promote nail health.
9. Nail Strengtheners
Consider using nail strengtheners or protective coatings designed to fortify and protect the toenails. These products can help reduce susceptibility to damage and promote nail resilience.
10. Monitor for Improvement
Keep track of any changes in the appearance or symptoms of your purple toenails. If you notice persistent discoloration, worsening pain, or signs of infection such as redness, swelling, or discharge, seek medical attention promptly.
Prevention Strategies
Taking proactive steps to prevent purple toenails is essential for maintaining foot health and avoiding discomfort. Here’s a detailed look at key preventive measures:
Footwear Selection:
- Choosing the right footwear is paramount to preventing toenail issues. Look for shoes that provide adequate room for your toes, allowing them to wiggle freely without feeling cramped. Look for styles with a wide toe box that accommodates the natural shape of your foot. Avoid shoes that constrict or rub against your toenails, as this can lead to irritation and bruising. When trying on shoes, ensure there is a thumb’s width of space between the tip of your longest toe and the end of the shoe. Additionally, opt for breathable materials to promote air circulation and reduce moisture buildup, which can contribute to fungal infections.
Proper Foot Care:
- Maintaining good foot hygiene is essential for preventing infections and toenail problems. Wash your feet daily with mild soap and warm water, paying attention to the areas between the toes and around the toenails. Dry your feet thoroughly, especially between the toes, to prevent fungal growth. Trim your toenails straight across with clean, sharp nail clippers to prevent ingrown toenails. Avoid cutting the nails too short or rounding the edges, as this can increase the risk of ingrown nails and toenail trauma. Moisturize your feet regularly to keep the skin soft and supple, focusing on the toenails and surrounding areas.
Regular Exercise:
- Incorporating regular exercise into your routine is essential for overall health and wellbeing. However, it’s crucial to choose low-impact activities and implement proper warm-up and cool-down routines to minimize the risk of toenail trauma. Engage in activities such as walking, swimming, or cycling, which provide cardiovascular benefits without placing excessive stress on the feet. Before starting any exercise session, perform dynamic stretches to warm up the muscles and increase blood flow to the toes. Afterward, cool down with static stretches to promote flexibility and prevent muscle tightness. Wearing appropriate footwear designed for your chosen activity can further reduce the risk of toenail injuries.
Conclusion
Purple toenails can be a source of concern, causing discomfort and prompting questions about their underlying causes. However, understanding the factors contributing to purple toenails and implementing preventive measures can help manage the condition effectively.
By taking proactive steps such as selecting appropriate footwear, practicing proper foot care, and engaging in safe exercise routines, you can significantly reduce the risk of developing purple toenails. These preventive measures not only promote foot health but also contribute to overall well-being.
If you find yourself troubled by purple toenails despite preventive efforts, don’t hesitate to seek guidance from a healthcare professional. They can provide personalized care and treatment options tailored to your specific needs and circumstances.
Remember, prioritizing foot health is essential for maintaining an active and comfortable lifestyle. By staying informed, proactive, and attentive to your foot care routine, you can enjoy healthier and happier feet for years to come.
Comprehensive Guide: How to Fix Curly Toe?
Curled toes, often stemming from neurological injuries like strokes, can significantly impact mobility and comfort. Understanding the types, causes, and effective treatments for curled toes is crucial for recovery. In this comprehensive guide, I’ll go into various methods to alleviate curled toes, catering to diverse needs and preferences.
Types of Curled Toes
Curled toes encompass several variations, each affecting different joints and toes. Understanding these types, including hammertoe, mallet toe, claw toe, and curly toe, lays the foundation for targeted treatment strategies.
Hammertoe
- Definition: Hammertoe occurs when the toe bends at the middle joint, causing the joint to point upward while the tip of the toe points downward. It commonly affects the second toe but can occur in any toe.
Mallet Toe
- Definition: Mallet toe is characterized by the downward bending of the toe at the joint closest to the tip of the toe. This condition primarily affects the second toe, leading to a deformity where the tip of the toe bends downwards.
Claw Toe
- Definition: Claw toe is a condition where the four smallest toes bend upward at the joint closest to the foot, while the remaining joints bend downward. This results in toes that appear to curl downward, with severe cases potentially curling into themselves.
Curly Toe
- Definition: Curly toe manifests as a downward and often sideways curling of the toe, typically occurring at birth. It commonly affects the third, fourth, or pinky toes, causing problems in approximately 10% of cases. Unlike other curled toes, curly toe may not always cause discomfort or require treatment.
Causes of Curled Toes
While curled toes can be congenital, neurological injuries, especially strokes, are common culprits. Post-stroke spasticity leads to involuntary muscle tightening, exacerbating curled toes. Recognizing these underlying causes is pivotal for effective treatment planning.
Treatments for Curled Toes
- Addressing curled toes necessitates a multi-faceted approach. From rehabilitative exercises to innovative interventions, a range of treatments offers hope for recovery post-stroke.
Rehab Exercises
- Tailored exercises play a pivotal role in retraining the brain and restoring toe mobility. These exercises harness neuroplasticity to promote recovery, offering a non-invasive yet potent solution.
Botox Treatment
- Botox injections effectively alleviate spasticity, facilitating relaxed and straightened toes. Backed by evidence, Botox emerges as a promising option for individuals grappling with curled toes post-stroke.
Electrical Stimulation
- Harnessing the power of electrical stimulation aids in re-establishing neural connections, bolstering the efficacy of rehabilitation efforts. When integrated with other modalities, it fosters comprehensive recovery.
Orthotic Support
- Orthotics provide invaluable support by aligning toes and alleviating discomfort. Customized orthotic solutions, coupled with diligent usage, promote long-term relief and enhance mobility.
Therapeutic Taping
- Innovative therapeutic taping techniques, coupled with professional guidance, facilitate optimal toe alignment and pain relief. This adjunct therapy empowers individuals in their journey towards curled toe correction.
Insoles and Toe Separators
- Simple yet effective, insoles and toe separators offer immediate relief by optimizing toe alignment. These cost-effective solutions augment treatment efficacy, promoting comfort and mobility.
Roomy Footwear
- Selecting footwear with spacious toe boxes is imperative for mitigating pressure and facilitating natural toe alignment. Avoiding restrictive footwear fosters comfort and accelerates recovery progress.
Surgical Intervention
- In severe cases resistant to conservative measures, surgical intervention may be warranted. While a last resort, surgical correction offers a viable solution for individuals grappling with persistent curled toes.
Exercises for Curled Toes
These exercises are not only instrumental in promoting physical rehabilitation but also play a crucial role in bolstering mental resilience. From simple toe taps to more advanced towel curls, each exercise is meticulously designed to target specific muscle groups, promoting toe mobility, and facilitating neural rewiring. By engaging in these exercises consistently, individuals not only strengthen the muscles surrounding the toes but also stimulate neuroplasticity, laying the groundwork for lasting improvement.
Here’s a step-by-step guide to fixing curled toes after a stroke:
Step 1: Consult with a Healthcare Professional:
- Schedule an appointment with a healthcare professional, preferably a doctor or therapist specializing in stroke rehabilitation.
- Discuss your symptoms, medical history, and concerns related to curled toes.
- Receive a thorough assessment to determine the underlying causes and severity of your condition.
Step 2: Understand the Types and Causes of Curled Toes:
- Educate yourself about the different types of curled toes, including hammertoe, mallet toe, claw toe, and curly toe.
- Learn about the potential causes of curled toes, such as neurological injuries like strokes and congenital factors.
Step 3: Explore Treatment Options:
- Work closely with your healthcare provider to explore various treatment options tailored to your specific needs and preferences.
- Discuss non-invasive treatments such as rehabilitative exercises, Botox injections, electrical stimulation, orthotic support, therapeutic taping, and lifestyle modifications.
- Consider the possibility of surgical intervention as a last resort for severe cases resistant to conservative measures.
Step 4: Implement Rehabilitative Exercises:
- Begin incorporating rehabilitative exercises into your daily routine to promote toe mobility and neural rewiring.
- Start with simple exercises like toe taps, floor grips, finger squeezes, marble pickup, and towel curls.
- Gradually increase the intensity and frequency of exercises as tolerated, aiming for consistent practice throughout the day.
Step 5: Follow Rehabilitation Guidelines:
- Adhere to any specific guidelines provided by your healthcare provider regarding exercise duration, intensity, and frequency.
- Seek guidance on proper technique to ensure maximum effectiveness and minimize the risk of injury.
- Monitor your progress closely and communicate any concerns or challenges with your healthcare team.
Step 6: Incorporate Lifestyle Modifications:
- Make necessary adjustments to your footwear, opting for shoes with spacious toe boxes to alleviate pressure and facilitate natural toe alignment.
- Embrace healthy lifestyle habits such as maintaining a balanced diet, staying hydrated, and engaging in regular physical activity to support overall recovery.
Step 7: Stay Patient and Persistent:
- Understand that recovery from curled toes after a stroke is a gradual process that requires patience and persistence.
- Celebrate small victories along the way and stay motivated by focusing on the progress you make, no matter how incremental.
- Reach out to your support network for encouragement and assistance whenever needed.
Step 8: Monitor Progress and Adjust Treatment Plan:
- Regularly assess your progress and communicate any changes or improvements with your healthcare provider.
- Adjust your treatment plan as necessary based on feedback from your healthcare team and evolving needs.
- Stay proactive in managing your recovery journey, advocating for yourself, and seeking additional support as needed.
Conclusion
Navigating curled toes post-stroke necessitates a holistic approach, encompassing targeted treatments, diligent exercises, and adaptive lifestyle adjustments. By leveraging diverse interventions and fostering proactive engagement, individuals can reclaim mobility and enhance their quality-of-life post-stroke. Consultation with healthcare professionals is paramount, ensuring personalized guidance tailored to individual needs. Embracing this comprehensive approach paves the path towards curled toe correction and empowers individuals in their journey towards recovery.
Your Complete Guide on How to Fix Dry Feet

Whether it’s the harsh winter weather or simply neglecting foot care, dealing with this common issue can be a nuisance. But fear not! We’ve compiled expert tips and advice to help you restore your heels to their soft and smooth glory.
Understanding the Causes of Dry Feet
Dry, cracked heels can stem from various factors, each requiring specific attention to effectively address the issue. Understanding these root causes is essential for tailoring your treatment and preventive measures. Here’s a closer look at each factor:
Dehydration:
- Lack of sufficient water intake can lead to overall dehydration, affecting skin health, including the heels.
- Dry environments, especially during winter or in arid climates, can further exacerbate dehydration and dryness.
- Solution: Increase water intake, use a humidifier in dry indoor environments, and moisturize regularly to replenish lost moisture.
Weather Conditions:
- Exposure to harsh weather elements, such as cold temperatures, wind, and low humidity, can strip moisture from the skin, leading to dry, cracked heels.
- Prolonged sun exposure without adequate protection can also contribute to dryness and damage.
- Solution: Wear protective footwear and moisturize exposed skin regularly, especially during extreme weather conditions.
Lack of Proper Foot Care:
- Neglecting foot hygiene and care routines, such as infrequent moisturizing or improper shoe choices, can contribute to dry, cracked heels.
- Failure to exfoliate regularly can allow dead skin cells to accumulate, leading to thickened, rough heels.
- Solution: Establish a daily foot care routine that includes gentle cleansing, moisturizing, and regular exfoliation to maintain healthy skin on your heels.
Underlying Medical Conditions:
- Certain medical conditions, such as diabetes, thyroid disorders, or psoriasis, can impair skin health and increase the risk of dry, cracked heels.
- These conditions may affect circulation, nerve function, or skin regeneration, leading to persistent dryness and skin damage.
- Solution: Consult a healthcare professional for proper diagnosis and management of underlying medical conditions contributing to dry, cracked heels. Follow their recommendations for treatment and preventive measures tailored to your specific health needs.
Hydration Matters
Hydration plays a crucial role in maintaining skin health, including the condition of your heels. Here’s why it’s important and how you can ensure adequate hydration:
Skin Barrier Function:
- The skin acts as a barrier, protecting the body from external threats like pathogens, chemicals, and environmental stressors.
- Adequate hydration is essential for maintaining the integrity of the skin barrier. When the skin lacks moisture, it becomes dry, tight, and more susceptible to damage.
Moisture Retention:
- Skin cells require water to function properly. Hydrated skin cells are plump and flexible, allowing them to retain moisture effectively.
- Proper hydration helps prevent water loss through the skin, keeping it supple and hydrated.
Skin Regeneration:
- Hydration supports the natural process of skin regeneration, where old, damaged skin cells are replaced by new ones.
- When the body is well-hydrated, skin regeneration occurs more efficiently, promoting healthier, smoother skin, including the heels.
Prevention of Dryness and Cracking:
- Dehydration can lead to dry, cracked skin, including on the heels. When the skin lacks moisture, it becomes dry and brittle, making it more prone to cracking and fissures.
- By staying hydrated, you help maintain the moisture balance in your skin, reducing the risk of dryness and cracking.
To ensure adequate hydration and promote healthy skin, follow these tips:
Drink Plenty of Water:
- Aim to drink at least eight glasses of water per day, or more if you’re physically active or in a hot climate.
- Water helps hydrate your body from the inside out, supporting overall skin health, including the skin on your heels.
Use a Humidifier:
- During dry seasons or in environments with low humidity, consider using a humidifier at home to add moisture to the air.
- A humidifier can help prevent excessive moisture loss from the skin, keeping it hydrated and less prone to dryness and cracking.
By prioritizing hydration through both internal and external measures, you can support the health and integrity of your skin, including your heels. Remember to drink water regularly, especially during dry seasons, and consider using a humidifier to maintain moisture levels in your home.
Gentle Cleansing
Choosing the right cleanser and being mindful of shower duration are essential steps in maintaining the health of your feet, particularly when dealing with dry, cracked heels.
Selecting a Gentle Cleanser:
- Go for a gentle, fragrance-free cleanser specifically formulated for sensitive skin when washing your feet.
- Fragrances and harsh chemicals in some soaps can strip away the natural oils from your skin, exacerbating dryness.
- Look for cleansers with moisturizing ingredients like glycerin or ceramides to help hydrate your skin while cleansing.
Limiting Shower Time:
- Keep showers brief, aiming for 5 to 10 minutes, to prevent excessive moisture loss from your skin.
- Prolonged exposure to hot water can strip away the skin’s natural oils, leading to dryness and irritation.
- Use lukewarm water instead of hot water, as it is less likely to cause drying of the skin.
Moisturize Regularly
Moisturizing is indeed essential for both healing existing dry, cracked heels and preventing their recurrence. Here’s why it’s crucial and how to do it effectively:
Importance of Moisturizing:
- Moisturizers help replenish the skin’s natural moisture barrier, preventing water loss and promoting hydration.
- For dry, cracked heels, moisturizing is particularly important as it helps soften rough skin, soothe irritation, and prevent further damage.
Choosing the Right Moisturizer:
- Look for moisturizers containing ingredients known for their hydrating properties, such as urea, glycerin, shea butter, or hyaluronic acid.
- These ingredients work to attract and retain moisture in the skin, effectively combating dryness and promoting healing.
Application Technique:
- Apply moisturizer immediately after bathing while your skin is still damp. This helps lock in moisture and allows the moisturizer to penetrate deeply into the skin.
- Use gentle, circular motions to massage the moisturizer into your heels, focusing on areas prone to dryness and cracking.
- Reapply moisturizer throughout the day as needed, especially after activities that may further dry out your skin, such as swimming or prolonged exposure to air conditioning.
Exfoliate
Regular exfoliation is a key step in maintaining soft, smooth heels by removing dead skin cells and promoting cell turnover.
Here’s why it’s important and how to do it safely:
Importance of Exfoliation:
- Over time, dead skin cells can accumulate on the surface of your heels, leading to dryness, roughness, and a dull appearance.
- Exfoliation helps slough off these dead cells, revealing newer, healthier skin underneath and improving the overall texture and appearance of your heels.
Choosing the Right Exfoliation Method:
- Opt for a gentle scrub or a pumice stone specifically designed for use on feet. These tools are effective at removing dead skin without causing irritation.
- Avoid harsh exfoliants or tools with rough textures, as they can damage the delicate skin on your heels and exacerbate dryness and cracking.
Exfoliation Technique:
- Before exfoliating, soak your feet in warm water for 10-15 minutes to soften the skin and make it easier to remove dead cells.
- Gently massage the scrub or pumice stone onto your heels using circular motions, focusing on rough or calloused areas.
- Be careful not to apply too much pressure or overdo it, as excessive exfoliation can cause irritation and damage to the skin.
- Limit exfoliation to 1-2 times per week to avoid overexposing your heels to the abrasive effects of exfoliants.
Post-Exfoliation Care:
- After exfoliating, rinse your feet thoroughly with warm water and pat them dry with a soft towel.
- Follow up with a moisturizer to hydrate and nourish the freshly exfoliated skin, helping to maintain its softness and prevent dryness.
By incorporating regular, gentle exfoliation into your foot care routine, you can effectively remove dead skin cells, promote cell turnover, and keep your heels soft, smooth, and healthy. Just remember to exfoliate mindfully and avoid overdoing it to prevent irritation and damage to the skin.
Protective Measures
Protecting your feet with the right footwear and regular moisturizing is crucial for preventing and alleviating dry, cracked heels. Here’s why and how to do it effectively:
Importance of Footwear:
- Supportive shoes and cushioned socks are vital for providing protection and reducing pressure on your feet, especially if you spend a lot of time standing or walking. Well-fitting shoes with proper support help distribute weight evenly, minimizing strain and reducing the risk of calluses and blisters.
Choosing Supportive Shoes:
- Go for shoes with cushioned insoles and adequate arch support to minimize impact and provide comfort. Avoid open-backed shoes like flip-flops or sandals, as they expose your heels to friction and dryness, potentially leading to irritation and cracking.
Moisturizing for Protection:
- Regularly moisturizing your feet creates a protective barrier, shielding them from harsh weather conditions such as cold temperatures, wind, and low humidity. Apply moisturizer daily, paying special attention to rough or cracked areas, to keep your skin hydrated and supple.
Additional Tips for Foot Care:
- Rotate your shoes regularly to allow them to air out and prevent moisture buildup, reducing the risk of fungal infections and foot odor. Consider wearing moisture-wicking socks made of breathable materials to keep your feet dry and comfortable throughout the day.
Seek Medical Advice
Knowing when to seek medical advice for dry, cracked heels is important to ensure proper treatment and management, especially if home remedies have not been effective. Here are some indicators that it may be time to consult a healthcare professional:
Persistent Symptoms:
- If your dry, cracked heels persist despite following home care remedies consistently for several weeks or months, it may indicate an underlying issue that requires medical attention.
Severe Pain or Discomfort:
- If you experience severe pain, inflammation, or discomfort in your heels, it could be a sign of an infection, nerve damage, or other serious condition that requires prompt medical evaluation.
Signs of Infection:
- Redness, warmth, swelling, or drainage from the cracks in your heels may indicate an infection. If you notice any of these symptoms, seek medical attention promptly to prevent complications.
Underlying Health Conditions:
- If you have underlying health conditions such as diabetes, peripheral artery disease, or autoimmune disorders, it’s important to consult a healthcare professional for specialized care and management of foot problems.
Difficulty Walking:
- If dry, cracked heels make it difficult for you to walk or perform daily activities, it’s essential to seek medical advice to address the underlying cause and prevent further impairment.
History of Skin Disorders:
- If you have a history of chronic skin conditions such as eczema, psoriasis, or dermatitis, your healthcare provider can provide tailored treatment options to manage your symptoms effectively.
Medication Side Effects:
- Certain medications can cause dry skin as a side effect. If you suspect that your dry, cracked heels may be related to medication you’re taking, consult your healthcare provider for guidance.
Conclusion
Should I Wear Compression Socks While Walking?

Walking is one of the simplest and most effective forms of exercise, offering numerous health benefits. But if you’ve ever wondered, should I wear compression socks while walking? the short answer is yes, you should consider it. Many walkers and runners alike are curious about the potential benefits and drawbacks of wearing compression socks during their routines. In this blog post, we’ll explore this topic in detail, covering the benefits, types, and specific considerations for various groups of people. Maximize Comfort – Get CopperZen Socks!
Benefits of Wearing Compression Socks for Walking
Compression socks are designed to apply gentle pressure to your legs, enhancing blood flow and providing numerous benefits, especially during physical activities like walking. Here are some key advantages of wearing compression socks while walking:
- Improved Circulation: Compression socks help promote better blood flow from your legs back to your heart. This enhanced circulation can prevent blood from pooling in your lower extremities, reducing the risk of conditions like deep vein thrombosis (DVT) and varicose veins. Improved circulation also ensures that your muscles receive more oxygen, which can boost overall walking performance.
- Reduced Muscle Soreness: By supporting your muscles and reducing the amount of muscle vibration during walking, compression socks can help decrease muscle soreness and fatigue. This is particularly beneficial after long walking sessions, as it helps in faster recovery and prepares your legs for the next walk.
- Prevention of Swelling: For those who experience swelling in their legs and feet, compression socks can help minimize this issue by preventing fluid buildup. This is especially important for individuals who are on their feet for extended periods or those who walk long distances.
- Support for Varicose Veins: If you have varicose veins, wearing compression socks can provide relief by reducing swelling and discomfort, and supporting the vein structure. This makes walking more comfortable and lessens the pain associated with varicose veins.
- Enhanced Endurance: When walking long distances, your legs endure significant stress and strain. Compression socks offer additional support, helping you maintain endurance and comfort. This is particularly beneficial for marathon walkers or those embarking on lengthy hikes, as it helps prevent common issues like swelling, muscle fatigue, and cramps.