feetcorrector
Baking Soda for Toenail Fungus Relief
Say Goodbye to Toenail Fungus Forever with These Baking Soda Hacks!
Are you looking for a simple and effective way to keep your toenails and feet clean and healthy? Look no further than your kitchen pantry! Baking soda, that versatile staple, can work wonders for your foot care routine. In this guide, we’ll explore various methods of using baking soda to clean your toenails and feet, providing easy-to-follow steps and highlighting the benefits of each approach. Let’s dive in

1. Baking Soda Soak:
- Benefits: Softens skin and toenails, neutralizes odor.
- How to do it: Fill a basin or tub with warm water and add 3-4 tablespoons of baking soda. Soak your feet for 15-20 minutes, then dry thoroughly.
2. Baking Soda Scrub:
- Benefits: Exfoliates dead skin cells, leaves feet feeling refreshed.
- How to do it: Mix baking soda with water to form a paste. Gently scrub onto your toenails and feet using a soft brush or washcloth, then rinse off.

3. Foot Odor Control:
- Benefits: Absorbs moisture, neutralizes odor.
- How to do it: Sprinkle baking soda directly into your shoes or socks to absorb moisture and neutralize odor-causing bacteria.
4. Toenail Brightening:
- Benefits: Brightens and whitens discolored toenails.
- How to do it: Mix baking soda with lemon juice to form a paste. Apply to toenails, let sit for a few minutes, then rinse off.

5. Athlete’s Foot Treatment:
- Benefits: Alleviates symptoms of athlete’s foot, helps maintain foot hygiene.
- How to do it: Create a foot bath with warm water and baking soda. Soak your feet for 15-20 minutes daily until symptoms improve.
6. Callus Softener:
- Benefits: Softens calluses, making them easier to remove.
- How to do it: Make a paste with baking soda and water. Apply to callused areas, cover with a warm, damp towel for 10-15 minutes, then gently remove calluses with a pumice stone or foot file.

7. Toenail Fungus Prevention:
- Benefits: Helps keep feet clean and dry, preventing fungal growth.
- How to do it: Incorporate baking soda foot soaks or scrubs into your hygiene routine to maintain clean, dry feet and prevent toenail fungus.
Conclusion
With baking soda as your secret weapon, achieving clean and healthy toenails and feet has never been easier. Whether you’re looking to soften skin, brighten toenails, or combat foot odor, there’s a baking soda solution for you. Incorporate these simple methods into your foot care routine and step into a world of clean, refreshed feet!
Step by Step Guide: How to Disinfect Nail Clippers from Fungus
The Ultimate Guide to Disinfecting Nail Clippers
Keeping our nail clippers clean and free from harmful bacteria is crucial for maintaining healthy nails and preventing infections. Whether you’re a professional nail technician or someone who likes to do their own manicures at home, knowing how to properly disinfect nail clippers is essential. In this post, we’ll explore the best methods and practices for ensuring your nail clippers are thoroughly disinfected.
Why Disinfecting Nail Clippers is Important
Nail clippers are commonly used to trim nails, which can harbor dirt, bacteria, and even fungal spores. When nail clippers are not properly disinfected, they can become a breeding ground for harmful pathogens, increasing the risk of infections such as nail fungus, bacterial infections, and even warts. This is especially concerning in environments like nail salons where multiple people may use the same tools.
Materials Needed
Before we dive into the methods, let’s gather the materials needed for disinfecting nail clippers:
- Nail clippers
- Rubbing alcohol or disinfectant solution
- Cotton balls or pads
- Clean towel or paper towels
- Small bowl or container (optional)
3 Simple Methods for Disinfecting Nail Clippers
There are several effective methods for disinfecting nail clippers. Here, we’ll discuss three commonly used techniques:
- Rubbing Alcohol Soak:
- Begin by rinsing the nail clippers under warm water to remove any visible debris.
- Pour rubbing alcohol into a small bowl or container, enough to fully submerge the nail clippers.
- Place the nail clippers into the alcohol solution and let them soak for at least 10 minutes to ensure thorough disinfection.
- After soaking, remove the nail clippers and wipe them dry with a clean towel or paper towel.
- Let the nail clippers air dry completely before using them again.
- Disinfectant Spray:
- Rinse the nail clippers under warm water to remove any debris.
- Spray a disinfectant solution directly onto the blades of the nail clippers, ensuring complete coverage.
- Let the disinfectant sit on the blades for the recommended amount of time as specified on the product label.
- Use a clean cotton ball or pad to wipe off any excess disinfectant.
- Allow the nail clippers to air dry completely before storing or using them.
- Boiling Water Method:
- Boil a pot of water on the stove.
- Once the water reaches a rolling boil, carefully place the nail clippers into the boiling water using tongs.
- Let the nail clippers boil for at least 10 minutes to ensure thorough disinfection.
- After boiling, remove the nail clippers from the water and allow them to cool down.
- Once cooled, dry the nail clippers with a clean towel or paper towel and let them air dry completely.
Tips for Maintaining Clean Nail Clippers
In addition to regular disinfection, here are some tips for maintaining clean nail clippers:
- Clean your nail clippers after each use by rinsing them under warm water and wiping them dry with a clean towel.
- Store nail clippers in a clean, dry place to prevent the growth of bacteria and fungi.
- Avoid sharing nail clippers with others to reduce the risk of cross-contamination.
- Replace nail clippers if they become rusty or damaged beyond repair.
Conclusion
Properly disinfecting nail clippers is essential for maintaining healthy nails and preventing infections. By following the methods outlined in this guide and incorporating good hygiene practices, you can ensure that your nail clippers remain clean and safe to use. Remember to regularly disinfect your nail clippers and follow the tips for maintaining clean tools to keep your nails healthy and beautiful.
Foot Troubles Poll: What’s Your Biggest Concern?
Why My Toenail Stop Growing?
Have you noticed a sudden halt in the growth of your toenails? While it may seem like a minor issue, changes in toenail growth can sometimes indicate underlying health concerns. Here are 12 signs that suggest it’s time to schedule an appointment with a dermatologist for a thorough evaluation.

1. Melanoma under nail (Acral Lentiginous Melanoma)
If you see a dark streak under your toenail that’s new or changing, it could be a sign of melanoma, a very serious type of skin cancer. Melanoma can grow under your toenails slowly or quickly. It’s important to tell a doctor right away if you notice any strange changes in your toenails, so they can check it out and help keep you healthy.
- What could be causing my toenails to stop growing? Melanoma could be causing the dark streak.
- Are these changes in my toenails normal? No, they could indicate melanoma, a serious skin cancer.
- What should I do if I notice a dark streak? See a dermatologist immediately for a skin cancer check.

2. Nail lifting up (Onycholysis)
If your nail starts to lift up, it might mean you have a fungal infection, psoriasis, or maybe you hurt it somehow. It’s a good idea to see a dermatologist, a doctor who knows a lot about skin, to find out what’s causing it. They can help figure out the problem and suggest ways to make your toenail healthy again.
- How can I differentiate between harmless changes and signs of a serious condition? A dermatologist can diagnose the cause.
- Can I manage lifting toenails on my own? It’s best to see a dermatologist for proper treatment.
- What treatments are available? Treatment depends on the cause and may include antifungal medication or addressing underlying conditions.

3. Infection around toenail (Paronychia)
If your toe looks red and swollen around the nail, it might mean there’s an infection. Infections can get worse if you don’t treat them quickly, so it’s important to see a doctor right away. They can give you medicine to help clear up the infection and make your toe feel better.
- What should I do if I have redness and swelling around a toenail? See a dermatologist for diagnosis and treatment.
- Can I treat it at home? Early-stage infections may respond to soaks and antibiotics, but severe cases require professional treatment.

4. Infection under toenail (Paronychia)
If you notice a greenish-black color under your toenail, it could be a sign of a bacterial infection. It’s important to get help from a doctor because these infections can get worse if left untreated. A doctor can give you medicine to help clear up the infection and keep your toenail healthy.
- What causes a greenish-black color under the toenail? Bacterial infection.
- Can the infection worsen? Without treatment, it may worsen and require more extensive treatment.
- How can I get rid of the pain and tenderness? Treatment by a dermatologist can alleviate symptoms and clear the infection.
5. Fingernail with pits (Pitting)
If you see dents in your toenails that look like little holes made by an icepick, it could be a sign of a disease called psoriasis. This is a condition that affects your whole body, not just your nails. It’s a good idea to see a dermatologist, a special doctor who knows about skin, to find out what’s going on. They can help you figure out if it’s psoriasis and what you can do to feel better.
- What diseases could be causing pits in my toenails? Psoriasis, atopic dermatitis, or alopecia areata.
- How can I get a proper diagnosis? Consult a dermatologist, who can diagnose and treat underlying conditions.

6. Yellow nail syndrome (Yellow Nail Syndrome)
If your toenails turn yellow, get thick, and stop growing, it might mean there’s something going on inside your body, like lung disease or rheumatoid arthritis. It’s important to see a doctor for a check-up to find out what’s causing it. They can help you figure out what’s wrong and what you can do to feel better.
- What underlying health issues could yellow, thickened toenails indicate? Lung disease, rheumatoid arthritis, or serious nail infections.
- Can I treat yellow nails at home? Treatment depends on the underlying cause and may require medical intervention.

7. Deep groove in toenail (Beau Lines)
If you see deep lines or gaps in your toenails, it could be because of things like having a fever, getting hurt, having chemotherapy, or feeling really stressed out. It’s important to talk to a doctor if you notice this, so they can take a look and see what’s going on. They can help figure out why it’s happening and what you can do to make your toenails better.
- What causes deep grooves in toenails? Factors like fever, injury, chemotherapy, or stress.
- How can I determine the cause of grooves in my toenails? Consulting a dermatologist or primary care doctor is recommended.

8. Thick, overgrown toenails (Onychogryphosis)
If your toenails get really thick and grow a lot, like a ram’s horn, it might mean there’s something going on, like psoriasis or problems with your blood circulation. It’s important to see a doctor or a foot doctor called a podiatrist to check it out. They can help figure out what’s causing it and what you can do to help your toenails.
- Why are my toenails thickening and overgrowing? It could be due to underlying conditions like psoriasis or circulation problems.
- How can I treat thickened toenails? Treatment may involve help from a podiatrist or dermatologist.

9. Spoon-shaped toenails (Koilonychia)
If your toenails are thin and shaped like a spoon, it could mean you don’t have enough iron in your body, or it might be a sign of other health issues. It’s important to see a doctor to find out what’s causing it. They can help figure out if it’s because of low iron or something else and give you the right treatment to help you feel better.
- What could cause thin, spoon-shaped toenails? Iron deficiency or other health problems.
- How can I get a proper diagnosis? Consult a healthcare professional for diagnosis and treatment.

10. Washboard toenails (Onychotillomania)
If you see grooves and ridges in your toenails, it could be because you’ve been picking at or pushing back your cuticles without realizing it. It’s a good idea to see a dermatologist, a doctor who knows about skin, to help you stop this habit. They can give you tips to take care of your nails and keep them healthy.
- Why do I have grooves and ridges in my toenails? It may be due to a habit of picking at or pushing back cuticles.
- Can a dermatologist help with this habit? Yes, a dermatologist can provide guidance to break the habit and promote healthy nail growth.

11. Curved toenails (Clubbing)
If your toenails start to curve, it might not always be a big problem, but it could be a sign of something happening inside your body. It’s important to see a doctor, like a dermatologist who knows about skin, to check it out. They can help figure out why your toenails are curving and if there’s anything else going on that needs attention.
- What could cause my toenails to curve downward? It may be harmless or indicative of underlying diseases affecting various organs.
- How can I determine the cause of curved toenails? Consult a dermatologist for evaluation and diagnosis.
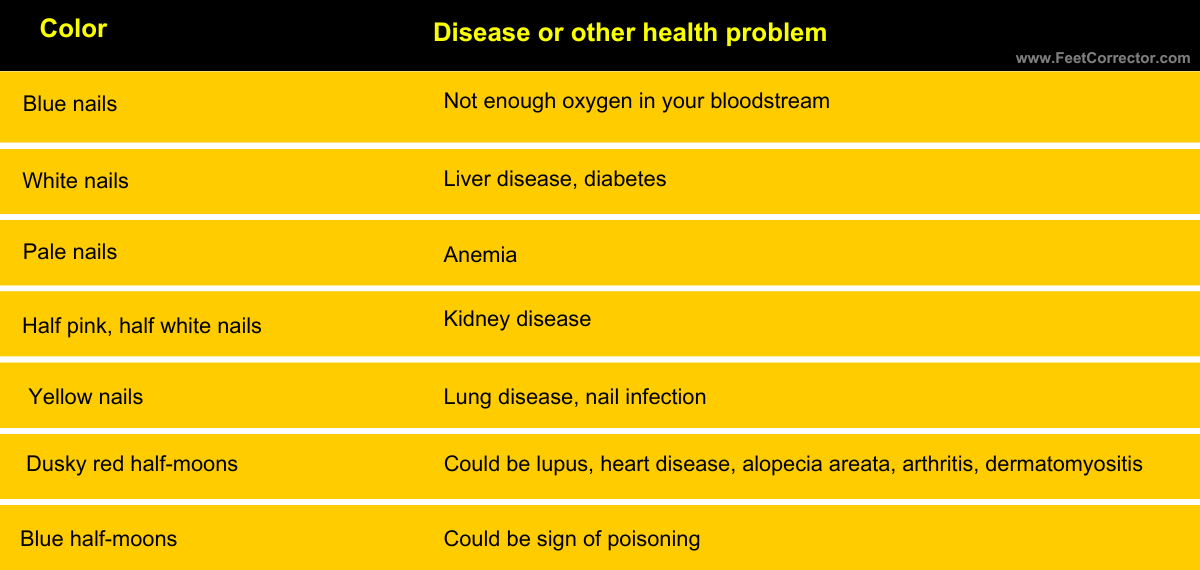
12. Color changes
If your toenails change color, it might mean something’s up with your health. For example, blue nails could mean you’re not getting enough oxygen, and yellow nails might signal lung disease or an infection. It’s important to see a doctor if you notice these changes, so they can figure out what’s causing it and help you feel better.
- What diseases could be indicated by changes in toenail color? Various diseases affecting organs like the liver, lungs, heart, or kidneys.
- Should I be concerned about changes in toenail color? Consult a dermatologist if you notice significant changes to your toenail color for proper evaluation.
While not every change in toenail growth is cause for alarm, it’s essential to pay attention to these signs and seek professional evaluation when necessary. A board-certified dermatologist can provide accurate diagnosis and recommend appropriate treatment to address any underlying issues affecting toenail growth.
Don’t ignore changes in your toenails; prioritize your foot health and schedule a consultation with a dermatologist if you notice any concerning signs mentioned above.
How To Treat An Abscess On Big Toe
Understanding and Addressing Abscesses on the Big Toe
You wake up one morning, ready to tackle the day ahead, only to find yourself hobbling in agony with every step you take. The culprit? An unexpected and excruciating pain radiating from your big toe. Abscesses on the big toe may seem innocuous at first glance, but beneath the surface lies a potentially perilous situation waiting to unfold. In this blog post, we’ll unravel the sinister origins, symptoms, and treatment strategies for abscesses on the big toe, empowering you to confront this menacing foe head-on.
Causes of Abscesses on the Big Toe
Abscesses on the big toe can stem from various factors, including:
- Ingrown Toenails: When the edge of the toenail grows into the surrounding skin, it can lead to irritation and inflammation, providing an entry point for bacteria to cause an abscess.
- Trauma: Injuries such as stubbing the toe or dropping heavy objects on it can break the skin, allowing bacteria to enter and form an abscess.
- Infections: Bacterial infections, particularly Staphylococcus aureus, can infiltrate the skin through cuts, scrapes, or open wounds on the toe, resulting in abscess formation.
- Poor Hygiene: Inadequate foot hygiene, including infrequent washing and wearing dirty socks or shoes, can contribute to bacterial growth and increase the risk of abscess development.
- Underlying Conditions: Certain skin conditions like dermatitis or psoriasis, as well as immunodeficiency disorders and diabetes, can make individuals more susceptible to abscesses on the big toe.
Symptoms of Abscesses on the Big Toe
Identifying the symptoms of an abscess on the big toe is crucial for prompt diagnosis and treatment. Common signs include:
- Pain and tenderness around the affected area
- Swelling, redness, and warmth
- Pus or discharge draining from the abscess
- Difficulty walking or wearing shoes comfortably
- Fever or chills in severe cases
Treatment Options for Abscesses on the Big Toe
Treating an abscess on the big toe typically involves a combination of home care and medical intervention:
- Warm Soaks: Soaking the affected foot in warm water several times a day can help alleviate pain and promote drainage of the abscess.
- Antibiotics: If the abscess is infected, your healthcare provider may prescribe antibiotics to target the underlying bacterial infection.
- Incision and Drainage: In cases where the abscess is large or does not improve with home care, a healthcare professional may need to make a small incision to drain the pus and relieve pressure.
- Surgical Intervention: For recurrent or severe abscesses, surgical procedures such as toenail removal or drainage may be necessary to prevent future occurrences.
Preventing Abscesses on the Big Toe
Taking proactive steps to maintain good foot hygiene and avoid common risk factors can help prevent abscesses on the big toe, these include:
- Trimming toenails straight across to prevent ingrown toenails
- Keeping feet clean and dry, especially between the toes
- Wearing well-fitting shoes and socks made of breathable materials
- Promptly treating any cuts, scrapes, or injuries to the feet
Conclusion
Abscesses on the big toe can be both painful and inconvenient, but with proper understanding and treatment, relief is within reach. By recognizing the causes, symptoms, and treatment options for abscesses on the big toe, you can take proactive steps to address this common foot ailment effectively. If you’re experiencing persistent or severe symptoms, don’t hesitate to seek medical attention for personalized care and guidance tailored to your needs.
Can Wearing Too Small Shoes Damage Your Toenails?
How To Cut Toenails That Are Very Hard, Long & Thick
A Complete Guide to Trimming Thick Toenails Safely and Effectively!
Dealing with thick toenails can be frustrating and uncomfortable, but fear not – you’re not alone. Whether it’s due to age, genetics, or underlying health conditions, many people face this issue. The key is to approach toenail trimming with care and the right techniques to ensure both comfort and safety.
Understanding Thick Toenails
Thick toenails, medically termed onychomycosis or fungal toenails can be a source of discomfort and self-consciousness for many individuals. This condition is often characterized by nails that become thickened, discolored, and brittle, making them difficult to trim and potentially leading to complications such as ingrown nails or infections.
Fungal infections thrive in warm, moist environments, making the feet an ideal breeding ground. These fungi can invade the nail bed and cause the nails to thicken, become discolored (usually yellow or brown), and develop a crumbly texture. Individuals who frequently wear tight-fitting shoes, engage in activities that cause excessive sweating, or have compromised immune systems are at higher risk of developing fungal toenail infections. No More Fungus! – Click Here To Learn More.
In addition to fungal infections, trauma to the toenails, such as repeated pressure or injury, can lead to thickening and deformity. Stubbing your toe, dropping heavy objects on your feet, or engaging in activities like running or dancing that put repetitive stress on the toenails can all contribute to this type of damage.
Genetics also play a significant role in nail health and thickness. Some individuals may inherit traits that predispose them to thicker nails, regardless of their lifestyle or environmental factors. Understanding your family history can provide valuable insight into the potential causes of thick toenails.
Certain underlying health conditions, such as psoriasis or diabetes, can also affect nail health and contribute to thickening. Psoriasis, an autoimmune disorder that causes rapid skin cell turnover, can affect the nails, leading to thickening, pitting, and discoloration. Diabetes, on the other hand, can cause peripheral neuropathy (nerve damage) and poor circulation, which can impact nail growth and increase the risk of fungal infections.
Regardless of the cause, it’s crucial to identify the underlying issue to effectively manage thick toenails. Treating the root cause, whether it’s addressing a fungal infection, managing chronic health conditions, or implementing preventive measures to reduce trauma, is essential for improving nail health over time. Consulting a healthcare professional, such as a podiatrist or dermatologist, can help diagnose the underlying cause and develop a personalized treatment plan tailored to your specific needs.
Preparation
Before diving into toenail trimming, gather the necessary tools:
- Nail clippers or scissors specifically designed for thick nails
- Emery board or nail file
- Warm water and mild soap for soaking
- Towel
- Antiseptic solution (optional)
Steps for Cutting Thick Toenails Safely
- Soften the nails: Soak your feet in warm, soapy water for about 10-15 minutes to soften the nails, making them easier to trim. Pat your feet dry afterward.
- Trim straight across: Use sharp, clean nail clippers or scissors designed for thick nails. Trim the nails straight across to prevent ingrown toenails. Avoid cutting the nails too short, as this can increase the risk of ingrown nails or infections.
- Smooth the edges: Use an emery board or nail file to gently smooth any rough edges or uneven surfaces. Be careful not to file too aggressively, as this can damage the surrounding skin.
- Maintain hygiene: After trimming, wash your feet with mild soap and water, then dry them thoroughly. Optionally, apply an antiseptic solution to prevent infection.
- Moisturize: Apply a moisturizing lotion or cream to keep the skin around the nails hydrated. This can help prevent dryness and cracking.
- Monitor for signs of infection: Keep an eye on your toenails for any signs of infection, such as redness, swelling, pain, or discharge. If you notice any abnormalities, consult a healthcare professional for proper evaluation and treatment.
Tips for Individuals with Limited Mobility
- Use a long-handled toenail clipper or seek assistance from a caregiver or podiatrist if reaching your feet is challenging.
- Consider visiting a podiatrist for professional toenail care if needed.
Conclusion
Trimming thick toenails requires patience, proper technique, and attention to detail. By following the steps outlined in this guide and maintaining good foot hygiene, you can keep your toenails healthy and comfortable. Remember to address any underlying health conditions contributing to thick toenails and seek professional help if necessary. With care and diligence, you can confidently tackle the task of toenail trimming and enjoy healthier feet.
Do You Have Cold Feet at Night? Here’s Why!
Understanding and Dealing with Cold Feet and Aching Legs at Night: Causes and Solutions
Do you find yourself battling not only cold feet but also aching legs when you’re trying to get some shut-eye? It’s a frustrating combination that can disrupt your sleep and leave you feeling restless. In this blog post, we’ll explore the causes behind cold feet and aching legs at night and offer practical solutions to help you find relief and enjoy more restful nights.
Understanding the Causes of Cold Feet at Night
Cold feet at night can be more than just a minor inconvenience; they can significantly disrupt your sleep and affect your overall comfort. To effectively address this issue, it’s crucial to understand the potential underlying causes. Here are the key factors that can contribute to cold feet at night:
- Poor Circulation: One of the primary reasons for cold feet at night is poor circulation. When you lie down to sleep, especially in a horizontal position, blood flow to your extremities, including your feet, may decrease. This reduction in blood flow can result from various factors, such as sitting or standing for prolonged periods during the day, leading to reduced circulation to the lower extremities. Additionally, certain medical conditions, like peripheral artery disease or diabetes, can impair circulation and contribute to cold feet.
- Room Temperature: The temperature of your sleeping environment plays a significant role in determining how warm or cold your feet feel at night. If your bedroom is too cold, your feet are more likely to become chilly, disrupting your ability to fall asleep or stay asleep comfortably. Conversely, excessively warm temperatures can also lead to discomfort and sweating, which may exacerbate issues like cold feet. Achieving the ideal room temperature for sleep, typically between 60 to 67 degrees Fahrenheit (15 to 20 degrees Celsius), can help promote better sleep quality and prevent cold feet.
- Underlying Medical Conditions: Cold feet at night can sometimes be a symptom of underlying medical conditions that affect circulation or nerve function. Conditions such as Raynaud’s disease, peripheral neuropathy, or hypothyroidism can cause cold extremities, including the feet, due to disruptions in blood flow or nerve signaling. If you experience persistent cold feet accompanied by other symptoms such as numbness, tingling, or discoloration, it’s essential to consult with a healthcare professional for proper evaluation and diagnosis.
Making Informed Decisions
Understanding the potential causes of cold feet at night empowers you to make informed decisions about how to address this issue effectively. By identifying the underlying factors contributing to your cold feet, you can implement targeted strategies to keep your feet warm and comfortable while you sleep. Here are some practical steps you can take:
- Improve Circulation: Incorporate regular exercise into your routine, elevate your feet when possible, and consider using compression socks to promote blood flow to your feet and legs.
- Optimize Room Temperature: Adjust your thermostat or use bedding layers to create a comfortable sleeping environment that keeps your feet at an ideal temperature for sleep.
- Monitor Symptoms: Pay attention to any additional symptoms or changes in your cold feet, such as numbness or pain, and discuss them with your healthcare provider to rule out underlying medical conditions.
- Invest in Warm Footwear: Choose appropriate socks and footwear that provide insulation and warmth, especially if you tend to have cold feet at night.
By addressing these factors and incorporating appropriate interventions, you can take proactive steps to mitigate cold feet at night and enjoy more restful and rejuvenating sleep. Remember that individual responses may vary, so it’s essential to find the strategies that work best for you and prioritize your overall sleep health.
Cold Ankles at Night
Cold ankles can accompany cold feet and may be caused by similar factors such as poor circulation or exposure to cold temperatures. Addressing the underlying causes of cold feet can also help alleviate cold ankles and promote better overall comfort during sleep.
Cold Feet and Hands at Night
If you experience cold feet and hands simultaneously at night, it could indicate issues with circulation or temperature regulation throughout your body. Implementing strategies to improve blood flow and maintain a comfortable sleeping environment can help prevent both cold feet and hands from disrupting your sleep.
Aching Legs at Night
Aching legs at night can have various causes, including muscle fatigue, overuse, or underlying medical conditions like restless leg syndrome or peripheral neuropathy. Identifying the root cause of your leg pain is essential for determining the most appropriate treatment and achieving relief.
Solutions for Cold Feet and Aching Legs
- Improve circulation through regular exercise, elevation, and massage techniques.
- Maintain a comfortable room temperature by adjusting your thermostat or using extra blankets.
- Choose appropriate bedding and clothing to keep your extremities warm and cozy.
- Practice relaxation techniques to reduce stress and promote relaxation before bedtime.
- Consult with a healthcare professional if you suspect underlying medical conditions contributing to your symptoms.
Conclusion
Cold feet and aching legs at night can be bothersome issues that interfere with your ability to get a good night’s sleep. By understanding the causes behind these symptoms and implementing practical solutions, you can minimize discomfort and enjoy more restful nights. Remember to prioritize your sleep hygiene and seek medical advice if you experience persistent or severe symptoms that impact your quality of life. With the right approach, you can conquer cold feet and aching legs and reclaim peaceful nights of slumber.
Watch This Video To Learn How To Stop Having Cold Feet!
Can Poor Circulation Lead to Toenail Problems?
Understanding Poor Circulation: Symptoms, Causes, and Treatment
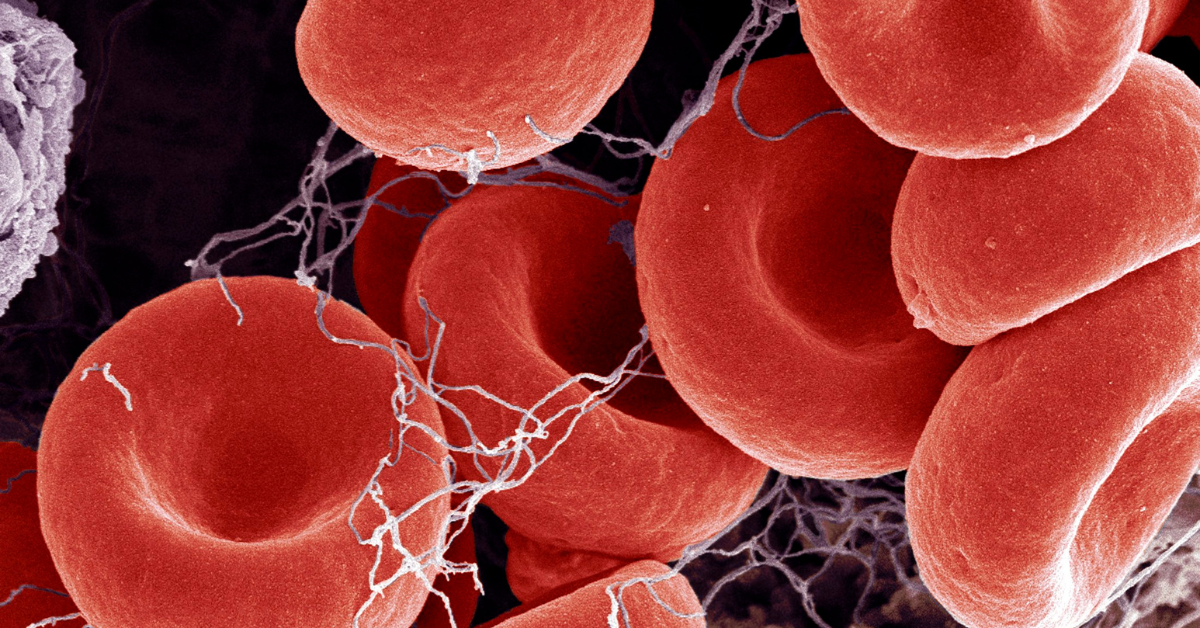
Poor circulation can indeed influence the health of your toenails. When blood flow to specific areas, such as the toes, is compromised, it can lead to various changes in the nails. Here’s why:
- Reduced Nutrient Supply: Your circulatory system plays a crucial role in delivering oxygen, nutrients, and essential building blocks to different parts of your body, including the nails. When blood flow diminishes, the nails receive fewer nutrients, affecting their growth and overall health.
- Brittle and Thickened Toenails: Poor circulation can cause toenails to become brittle and thicker. The lack of adequate oxygen and nutrients affects the nail matrix (the tissue responsible for nail growth), leading to alterations in nail texture and appearance.
- Color Changes: In some cases, poor circulation may cause toenails to change color. They might appear pale or even develop a bluish tint due to insufficient blood flow.
- Slowed Growth: Toenails with poor circulation tend to grow more slowly. If you’ve noticed that your toenails haven’t been growing as they should, it could be related to compromised blood flow.
- Risk of Infections: When circulation is impaired, minor wounds or injuries around the toenails may heal more slowly. This delay in healing increases the risk of infections. For example, ingrown toenails or small cuts can become problematic due to reduced blood flow, potentially leading to complications like gangrene.
- Peripheral Artery Disease (PAD):
- PAD is a condition characterized by narrowed arteries, particularly affecting the legs and feet.
- Plaque buildup in the arteries reduces blood flow, leading to poor circulation.
- As a result, toenails may suffer from inadequate nutrient supply and slower growth.
- Treating PAD is essential to address toenail-related issues caused by poor circulation.
Remember that toenails that stop growing or exhibit changes due to poor circulation should prompt you to seek medical attention. If you suspect that peripheral artery disease (PAD) is affecting your toenails, consult a vascular doctor promptly. Early intervention can prevent severe complications and promote overall circulatory health.
Symptoms of Poor Circulation
When blood flow to specific areas diminishes, you may encounter the following symptoms:
- Tingling and Numbness: A sensation of pins and needles in your limbs, especially the toes and fingers.
- Throbbing or Stinging Pain: Pain that feels like throbbing or stinging, often affecting the legs and feet.
- Muscle Cramps: Cramps in your muscles due to inadequate blood supply.
- Unique Symptoms: Depending on the underlying cause, additional symptoms may arise. For instance, individuals with peripheral artery disease (PAD) might also experience erectile dysfunction along with typical pain, numbness, and tingling.
Causes of Poor Circulation
Several factors contribute to poor circulation:
- Peripheral Artery Disease (PAD):
- PAD results from plaque accumulation in the arteries, narrowing them and reducing blood flow.
- Arteries stiffen due to atherosclerosis, leading to decreased circulation in the legs and feet.
- Symptoms include numbness, weakness, pain, and swelling.
- Thick Toenails: PAD can even affect toenail growth. Reduced blood flow prevents normal nail growth, causing thickened toenails1.
- Toenail Fungus: Interestingly, there’s a correlation between toenail fungus and reduced blood flow. Increasing circulation may help combat toenail fungus2.
- Blood Clots:
- Blood clots partially or entirely block blood flow.
- Clots in the arms or legs lead to circulation problems, causing pain, numbness, and weakness.
Treatment and Outlook
- Address the Underlying Cause:
- Treating the root cause is essential. Lifestyle changes, exercise, and dietary adjustments can improve circulation.
- Consult a healthcare professional promptly if you experience symptoms of poor circulation.
- Preventive Measures:
- Maintain a healthy lifestyle: Exercise regularly, quit smoking, and manage weight.
- Stay hydrated and consume a balanced diet rich in nutrients.
- Elevate your legs periodically to encourage blood flow. Click here to try these amazing medical socks for blood circulation!
- Medical Interventions:
- Medications, angioplasty, or bypass surgery may be necessary for severe cases.
- Consult a doctor for personalized recommendations.
Seeking medical advice from a healthcare professional is crucial for accurate diagnosis and personalized care. Your circulatory health matters, so take proactive steps to maintain optimal blood flow!
Big Blister on Big Toe: Causes, Treatment, and Prevention
Dealing with a Big Blister on Your Big Toe: Causes, Treatment, and Prevention
Having a big blister on your big toe can be more than just a nuisance—it can throw a wrench into your daily routine.
Whether you’re an avid hiker, a runner, or simply someone who enjoys comfortable footwear, dealing with a blister can be downright frustrating. But fear not! You’ve landed in the right spot.
In this blog post, we’ll get into the world of big toe blisters, exploring their causes, effective treatments, and smart strategies to prevent them from making an unwelcome return.
Why Do Big Toe Blisters Happen?
1. Friction Blisters:
- The most common culprit behind big toe blisters is friction. When your big toe rubs against a sock or shoe for an extended period, it can lead to the formation of these fluid-filled sacs.
- Picture those painful bubbles on your skin—clear, filled with serum, and determined to make their presence known.
2. Excessive Cold Exposure:
- Frostbite isn’t just a winter tale—it can cause blisters too. When your toes endure extreme cold, frostbite sets in, and blisters may follow suit.
- These blisters, often filled with clear or milky liquid, demand immediate attention to prevent further damage.
3. Insect Bites and Other Irritants:
- Bug bites, sun exposure, and excessive moisture—oh my! These irritants can also trigger toe blisters.
- While not everyone reacts the same way, some lucky individuals find themselves with blisters as an unexpected souvenir.
4. Blood Blisters:
- Blood blisters on the toes occur when a blister forms and blood vessels underneath become damaged, leading to blood leaking into the blister.
- These blisters appear either dark red or purple in color.
5. Sesamoiditis:
- Sesamoiditis occurs when the tendons around the sesamoid bones below the big toe become inflamed or irritated.
- Common in runners and ballet dancers, it causes discomfort and may require specific care.
Friction Blisters:
Friction blisters are the result of repetitive rubbing or friction against the skin, often caused by ill-fitting shoes or socks. When your big toe experiences prolonged friction, it can lead to the formation of these painful fluid-filled sacs. Here’s what you can do if you’re dealing with friction blisters:
- Proper Footwear Selection: Invest in well-fitting shoes with ample room in the toe box to reduce friction against your big toe. Look for shoes made from breathable materials like leather or mesh to minimize moisture buildup.
- Moisture-Wicking Socks: Opt for moisture-wicking socks to keep your feet dry and reduce friction. Look for seamless socks or double-layer socks to further minimize rubbing against your skin.
- Blister Prevention Products: Consider using blister pads or moleskin on areas prone to friction to provide additional cushioning and protection. Apply these products before engaging in activities that may exacerbate blister formation.
- Proper Hygiene: Keep your feet clean and dry to reduce the risk of infection. Wash your feet regularly with soap and water, and avoid wearing damp socks or shoes for extended periods.
- Treatment: If a friction blister does develop, avoid popping it unless absolutely necessary, as this can increase the risk of infection. Instead, clean the area gently with soap and water and apply a sterile bandage or blister pad to protect the blister while it heals.
Excessive Cold Exposure Blisters:
Blisters resulting from excessive cold exposure, such as frostbite, can be particularly painful and require immediate attention. Here’s what you should do if you suspect cold exposure has caused blisters on your toes:
- Gradual Rewarming: If you suspect frostbite, gradually rewarm the affected toes using warm (not hot) water or body heat. Avoid rubbing or massaging the area, as this can cause further damage to the skin.
- Protective Dressing: Once the toes have been rewarm, apply a sterile dressing to protect the blisters and prevent further trauma. Avoid popping the blisters, as they serve as a natural barrier against infection.
- Seek Medical Attention: If you experience severe pain, numbness, or discoloration of the toes, seek medical attention immediately. Frostbite can cause permanent damage to the skin and underlying tissues if not treated promptly.
Insect Bites and Other Irritants:
Insect bites, sun exposure, and other irritants can also trigger blisters on the toes, albeit less commonly. If you find yourself with blisters as an unexpected souvenir from these irritants, here’s what you can do:
- Preventive Measures: Take steps to avoid insect bites by using insect repellent, wearing protective clothing, and avoiding areas known for high insect activity. Similarly, protect your feet from excessive sun exposure by wearing sunscreen and seeking shade when possible.
- Prompt Treatment: If you do experience insect bites or sunburn on your toes, take prompt action to soothe the affected area. Apply a cold compress to reduce swelling and discomfort, and use over-the-counter antihistamines or anti-inflammatory creams to alleviate itching and inflammation.
- Avoid Scratching: Resist the urge to scratch the affected area, as this can further irritate the skin and increase the risk of infection. Instead, gently cleanse the area with soap and water and apply a soothing lotion or cream to promote healing.
- Monitor for Infection: Keep an eye on the blisters for signs of infection, such as increased redness, swelling, or pus discharge. If you suspect an infection, seek medical attention promptly for appropriate treatment.
Blood Blisters:
Blood blisters on the toes occur when a blister forms and blood vessels underneath become damaged, leading to blood leaking into the blister. Dealing with blood blisters requires special care to prevent infection and promote healing:
- Protective Measures: Avoid popping blood blisters, as this can increase the risk of infection and slow healing. Instead, cover the blister with a sterile bandage or blister pad to protect it from further trauma.
- Monitor for Complications: Keep an eye on the blood blister for signs of infection or worsening symptoms. If the blister becomes increasingly painful, red, or swollen, seek medical attention for evaluation and treatment.
- Pain Management: If the blood blister is causing discomfort, you can take over-the-counter pain relievers such as ibuprofen or acetaminophen to alleviate pain and reduce inflammation.
- Prevention: To prevent blood blisters from recurring, take steps to reduce friction and pressure on your toes. Wear properly fitting shoes and moisture-wicking socks, and use protective padding or cushioning as needed.
Sesamoiditis:
Sesamoiditis, inflammation of the tendons around the sesamoid bones below the big toe, can be a source of significant discomfort, particularly for runners and ballet dancers. If you’re dealing with sesamoiditis-related blisters, here are some strategies to manage the condition:
- Rest and Immobilization: Rest the affected foot and avoid activities that exacerbate the pain and inflammation associated with sesamoiditis. Consider using crutches or a walking boot to reduce weight-bearing on the affected area and promote healing.
- Ice Therapy: Apply ice packs or cold compresses to the painful area for 15-20 minutes several times a day to reduce pain and inflammation. Be sure to wrap the ice pack in a cloth to prevent frostbite and avoid direct contact with the skin.
- Padding and Support: Use cushioning insoles or pads to offload pressure from the sesamoid bones and provide support to the arch of the foot. Custom orthotics may also be helpful in redistributing pressure and reducing strain on the affected area.
- Stretching and Strengthening Exercises: Perform gentle stretching exercises to improve flexibility in the muscles and tendons surrounding the big toe. Additionally, incorporate strengthening exercises to improve stability and reduce strain on the sesamoid bones.
- Footwear Modification: Choose footwear with a wide toe box and adequate arch support to accommodate the shape of your foot and reduce pressure on the sesamoid bones. Avoid high-heeled shoes or shoes with thin, rigid soles that can exacerbate symptoms.
- Medical Treatment: If conservative measures fail to provide relief, consult a healthcare professional for further evaluation and treatment options. Depending on the severity of your symptoms, your doctor may recommend corticosteroid injections, physical therapy, or even surgical intervention to alleviate pain and restore function.
By implementing these strategies and working closely with your healthcare provider, you can effectively manage sesamoiditis-related blisters and reduce the impact of this condition on your daily activities.
Treatment and Pain Relief
Treatment for each type of blister varies based on its cause and severity. Let’s break down the treatment options for each:
1. Friction Blisters:
- Clean the affected area gently with soap and water.
- Apply a blister pad or moleskin to cushion the area and reduce friction.
- Avoid popping the blister unless it is large, painful, or likely to rupture on its own. If you must pop it, use a sterilized needle, and gently drain the fluid while leaving the overlying skin intact.
- Keep the area clean and dry to prevent infection.
- If the blister becomes infected or doesn’t heal, seek medical attention.
2. Excessive Cold Exposure Blisters:
- Gradually warm the affected toes using warm water (not hot) or body heat.
- Avoid rubbing or massaging the affected area, as this can cause further damage.
- Apply a sterile dressing to protect the blister and keep it clean.
- Seek medical attention if the blister is severe or if you suspect frostbite.
3. Insect Bites and Other Irritants:
- Clean the area with soap and water to remove any irritants.
- Apply a cold compress to reduce swelling and discomfort.
- Use over-the-counter antihistamines or anti-inflammatory creams to alleviate itching and inflammation.
- Avoid scratching the affected area to prevent further irritation and potential infection.
4. Blood Blisters:
- Refrain from popping the blister, as this can increase the risk of infection and slow healing.
- Protect the blister with a sterile bandage or blister pad to prevent further trauma.
- If the blister ruptures on its own, clean the area gently with soap and water and apply an antibiotic ointment.
- Seek medical attention if the blister is large, painful, or shows signs of infection.
5. Sesamoiditis:
- Rest the affected foot and avoid activities that aggravate the condition.
- Apply ice packs to reduce pain and inflammation.
- Use cushioning insoles or pads to relieve pressure on the sesamoid bones.
- Stretch and strengthen the muscles around the big toe to improve stability and reduce strain on the affected area.
- In severe cases, your doctor may recommend physical therapy, custom orthotics, or even surgery to alleviate symptoms and prevent further damage.
Preventing Future Blisters
Footwear:
- Invest in Properly Fitting Shoes: Ill-fitting shoes are a prime culprit for toe blisters. Ensure your shoes have enough room in the toe box to prevent rubbing and friction against your big toe. Consider visiting a shoe store with knowledgeable staff who can help you find the right fit for your foot shape and activity level.
- Choose Quality Materials: Opt for shoes made from breathable materials like leather or mesh to allow for better airflow and reduce moisture buildup, which can contribute to blister formation.
- Consider Activity-Specific Shoes: Different activities may require different types of footwear. For example, if you’re a runner, invest in running shoes designed to provide adequate support and cushioning for your feet, reducing the risk of blisters during your runs.
Sock Selection:
- Moisture-Wicking Socks: Moisture-wicking socks help to keep your feet dry by pulling moisture away from the skin. This can prevent excessive sweating, which can lead to friction and blister formation. Look for socks made from synthetic materials like polyester or merino wool, which are known for their moisture-wicking properties.
- Seamless Socks: Seamless socks can also help reduce friction and irritation, especially for individuals prone to blisters. Look for socks with flat seams or consider wearing double-layer socks to minimize rubbing against your skin.
Break-in Gradually:
- Take your time breaking in new shoes to allow your feet to adjust gradually. Start by wearing them for short periods around the house before venturing outside for longer walks or runs. This gives the shoes a chance to mold to your feet and reduces the likelihood of developing blisters from stiff or poorly fitting footwear.
Sun Protection:
- Don’t forget to protect your toes from the sun’s harmful rays! Apply sunscreen to exposed areas of your feet, including your toes, before heading outdoors, especially during prolonged periods of sun exposure. Look for a broad-spectrum sunscreen with an SPF of 30 or higher and reapply regularly, especially if you’re sweating or swimming.
By following these tips for footwear selection, sock choice, gradual break-in of new shoes, and sun protection for your toes, you can significantly reduce your risk of developing painful blisters on your big toe. Remember, prevention is key, so take proactive steps to keep your feet happy and blister-free.